Hair shedding is a common symptom of hypothyroidism, so ordering thyroid-stimulating hormone screening may be useful, Dr. Hordinsky said. Other tests that may offer clues are a complete blood count, ferritin measurement, and antinuclear antibody, as well as measuring for abnormal levels of vitamins D and E, thiamine, zinc, and total protein, she noted.
There are a number of inflammatory alopecias, Dr. Hordinsky said. Cicatricial alopecia presents with scalp scarring and hair loss. The inflammatory processes in cicatricial alopecia may be lymphocytic or neutrophilic. Lichen planopilaris is a common lymphocytic alopecia that presents with a red, itchy, burning scalp. The inflammatory process presents at the bulge region where the stem cells are located. Treatments include topical corticosteroids, intralesional corticosteroids, and topical nonsteroidal antiinflammatory drugs, as well as oral medications such as hydroxychloroquine, low-dose antibiotics, and corticosteroids.
Standard treatments for noninflammatory alopecia include minoxidil, which may be oral or topical. Hair-replacement surgery is another option, as are newer laser combs and low-level laser therapy, the latter of which has shown promise, Dr. Hordinsky said. Cosmetic interventions include shampoos or other hair-care products that help hair appear thicker.
Examine for Patterns
It’s important to examine the pattern of the hair loss on the scalp, Dr. Hordinsky said. Rheumatologists may see telogen effluvium in patients with chronic cutaneous lupus and especially in those with discoid lupus, whose hair loss often is seen at the crown of the head, Dr. Hordinsky said. In SLE, hair loss may be all over the scalp. In a female with perifollicular inflammation, scarring may progress from front to back on the scalp, she said. Frontal fibrosing alopecia (FFA) is a condition presenting with scarring and hair loss at the forehead that occurs most commonly in postmenopausal females. Newer therapies for FFA include anti-androgen therapy and pioglitazone (Actos), which is widely used for type II diabetes, she said.
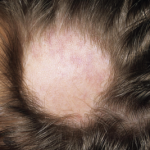
Alopecia areata, an autoimmune disease presenting with anagen effluvium, may be connected to RA based on data from genome-wide studies, Dr. Hordinsky said. Currently, there is no U.S. Food and Drug Administration–approved treatment for AA. In patchy AA or ophiasis AA, marked by hair loss at the circumference of the scalp, potential treatments include corticosteroids, minoxidil, anthralin (Psoriatec), and steroid shampoos. Treatments may include corticosteroids such as intralesional kenalog at 4 ccs injected at a 45-degree angle at the site of the hair loss every six weeks. “What is much more challenging is when alopecia areata is much more extensive and occurs all over the body,” she noted. In conditions like alopecia areata totalis or universalis, corticosteroids may also be used as well as immunotherapies like methotrexate, cyclosporine, sulfasalazine, or biologic drugs. In such cases, “we will do a scalp biopsy in our clinic, but the hair follicles are so small that they are barely visible,” Dr. Hordinsky said.