Cellular therapy refers to the use of live cells to replace or repair a damaged organ system. The first widespread use of this approach occurred more than 50 years ago when hematopoietic stem cells (HSCs) from the bone marrow of a healthy donor (allogeneic) were used to replace the hematopoietic system of a recipient after it was ablated during chemo/radio therapy of leukemia, the recipient’s hematopoietic system being “collateral damage” during the eradication of the unwanted leukemia cells.
This approach was later extended to the use of autologous stem cells in various malignant conditions such as breast cancer, allowing the use of more intense chemotherapy. In this context, the therapy is referred to as “hematopoietic stem cell support.” This principle was adopted for treating severe autoimmune disease more than 10 years ago in patients who failed to respond to conventional immunosuppression but in whom the marrow toxicity restricted dose escalation. Over 1,000 autoimmune disease patients have been treated, with around 30% achieving sustained remission.
Recently another cell, the mesenchymal stem cell (MSC), has been applied to the treatment of autoimmune disease. The concept is completely different from HSC in that pretreatment with chemotherapy is not required, and the MSCs are thought to home in on damaged tissue and exert a local paracrine healing effect. This article will review the basis of this novel treatment and results of recent trials.
Adult Stem Cells
A typical adult stem cell is one which, on division, results in one daughter cell that can further differentiate and replenish a whole compartment or tissue, while the other remains fully “stem” and self-renewing. This is called asymmetric division, and the stem cell is known as multipotent. (See Figure 1, p. 21.)
The best-studied example of this type of adult stem cell is the hematopoietic stem cell, which produces a trillion differentiated blood cells per day for the life of the animal. This remarkable property is possible because of a complex interaction between the stem cell and other cells and structures within the bone marrow microenvironment called the niche. However, other stem cells exist in the embryo from the moment of conception; the first eight to 16 divisions produce totipotent stem cells by symmetrical division. The word totipotent is used here because each cell may produce a full individual animal because the placental elements are present. Identical twins are the best example. Once the blastocyst has formed with an inner cell mass (destined to become the fetus) and an outer membrane (the early placenta), then the embryonal stem cells (ESCs) from the inner cell mass are called pluripotent. This means that all organs and tissues may be produced but no longer an intact individual. (See Figure 2, p. 22.)
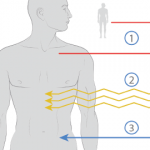
Recently, another cell, the mesenchymal stem cell (MSC), has been applied to the treatment of AD. The concept is completely different from HSC in that pretreatment with chemotherapy is not required, and the MSCs are thought to home in on damaged tissue and exert a local paracrine healing effect.
ESCs have extensive plasticity in terms of potential in vitro tissue differentiation, but they also carry an intrinsic risk of developing teratomas. In addition, the harvesting of pluripotent ESC requires destruction of an embryo, which raises ethical and theological issues limiting their utility.