HSCT is associated with substantial morbidity and mortality. In the beginning, transplant-related mortality for patients with systemic sclerosis (SSc) undergoing HSCT was higher than 10% in retrospective database analyses. In the last years, transplant-related mortality seems to be reduced after patients with advanced organ damage have been excluded from transplantation. Currently, active prospective trials recruit patients with a high risk of an adverse outcome of their autoimmune disease but with a still preserved organ function.
Toxicity of HSCT comes from the induction regimen itself. For example, cyclophosphamide or melphalan are potentially cardiotoxic, especially if used in patients with preexisting heart disease; this can be the case in autoimmune diseases such as SSc. G-CSF used to mobilize stem cells and to shorten engraftment after transplantation has been shown to induce a flare of the autoimmune disease in single cases. Antithymocyte globulin (ATG) used in the conditioning regimen is associated with hypersensitivity reactions.
The desired immunoablative effect of HSCT, on the other hand, comes along with an increased susceptibility to infections. This is the case mostly for bacteria or fungi during aplasia (up to 14 days after induction therapy), and this is also the case during the phase of immune reconstitution that can be delayed up to several months. During the latter, the patients are at risk for opportunistic infections or reactivation of silent viruses.
Results of HSCT for Autoimmune Diseases
Data on the effect of HSCT on patients suffering from autoimmune diseases are obtained from retrospective case series, the EBMT/European League Against Rheumatism (EULAR) database, and from published phase I/II trials.
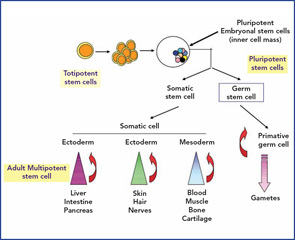
Up until March 2008, the EBMT/EULAR database included results from nearly 1,000 patients who received an HSCT for the indication autoimmune disease registered. Among these patients, more than 900 received an autologous HSCT and around 50 an allogeneic HSCT. Indication for autologous HSCT have been multiple sclerosis (MS) in 353 patients, SSc in 176, systemic lupus erythematosus (SLE) in 85, rheumatoid arthritis in 86, and other autoimmune diseases in fewer patients. (See Table 1, below left.) Most often, peripheral blood stem cells have been used as a stem-cell source but, in 65 cases, bone marrow was used. In more than one-third of the patients, in vitro CD34 positive selection had been performed.