In the two murine models of experimental autoimmune encephalomyelitis, both clinical and histological improvement occurred. However, in a murine model of arthritis, collagen induced arthritis was not improved by the addition of MSCs and the in vitro immunosuppressive effects were reversed by the addition of tumor necrosis factor-α. MSCs were not found in the joints. A second murine arthritis model showed, however, a positive outcome.
Recently, a murine model of streptozocin-induced diabetes mellitus was reported to improve clinically following transplantation with a combination of bone marrow derived cells and syngeneic and allogeneic MSCs following sublethal irradiation. The proposed mechanism was regeneration of recipient derived islet cells plus immunosuppression of autoreactive T cells. Neither cell product alone was effective.
MSCs and Human Experience
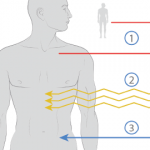
Ex vivo–expanded allogeneic MSCs have been infused in several phase I studies. No adverse events during or after MSC infusion have been observed, and no ectopic tissue formation has been noted. After infusion, MSCs remain in the circulation for no more than an hour. In another study, infusion of haploidentical MSCs to a patient with steroid-resistant severe acute GvHD of the gut and liver promptly improved liver values and intestinal function.
The EBMT is currently running protocols for prevention and treatment of acute GvHD through its developmental committee, and interim results of the treatment trial have recently been published. Thirty out of 55 steroid-resistant acute-GvHD patients had a complete response with no immediate toxicity.13
Autologous bone marrow derived MSCs have been shown to be potently antiproliferative to stimulated T cells from normal subjects and autoimmune (e.g., RA, SSc, Sjögren’s, SLE) patients; in SSc patients, these MSCs were normal in respect to proliferation, clonogenicity, and differentiation to bone and fat.14,15
Currently, few peer-reviewed publications concerning the results of using of MSCs in human autoimmune disease are available. There are several ongoing phase I/II clinical trials in autoimmune disease including MS, with discussions underway concerning other trials for other autoimmune disease such as type 1 diabetes mellitus, SSc, vasculitis, and SLE.
Important is the setting of clear therapeutic targets and harmonization of cell products, especially MSC source and type (autologous or allogeneic), cell expansion conditions, and trial protocols. In addition, long-term safety data collection across disciplines is required, and an international interdisciplinary registry of MSC-treated patients has been launched.
Summary
Cellular therapy using hematopoietic stem cells to support the ablated normal blood cells has enabled crossing a threshold of immunoablation, and early results suggest that a “resetting” of the immune system in patients with autoimmune disease beyond just immunosuppression is possible. Only phase III randomized trials will establish the true value of this approach. In contrast to the goals of treatment with HSC, MSCs are being used as “homing and healing” cells in various severe inflammatory settings including autoimmune disease, with phase I/II studies beginning. Importantly, no patient conditioning is required. Certainly, for diseases such as SSc where existing immunosuppressive has not been highly effective, stem-cell therapy may offer a fundamentally new approach to correct immune abnormalities and initiate repair. Although much work on stem cells needs to be performed in both the clinical and laboratory, there is strong optimism that a potential new era of therapy is now at hand.