Humoral immune and autoimmune responses result from either long-lived antibody secreting cells in specialized niches or novel stimulation of mature B cells such that they differentiate into antibody secreting cells. Currently, investigators lack effective tools to detect and isolate these autoreactive B cells for characterization.
Humoral immune and autoimmune responses result from either long-lived antibody secreting cells in specialized niches or novel stimulation of mature B cells such that they differentiate into antibody secreting cells. Currently, investigators lack effective tools to detect and isolate these autoreactive B cells for characterization.
New research suggests a combined strategy for detecting autoreactive B lymphocytes and/or antibody secreting cells may aid in choosing therapies that block B cells, plasma cells or both. The research by Raquel de la Varga-Martinez, a graduate student in immunology at the Hospital Universitario Puerta del Mar, Spain, and colleagues also points to a new tool for monitoring residual autoimmune disease. The results of the study were published online March 20 in the European Journal of Immunology.1
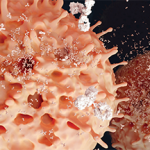
The study focused on patients with systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Researchers began by enriching B lymphocytes from the peripheral blood of patients using magnetic selection for extractable nuclear antigen and citrullinated peptide-bound immunobeads. The researchers found 75% of patients with SLE and 66% of patients with RA had autoreactive B lymphocytes in their blood. Additionally, they confirmed these B cells were truly autoreactive and recognized the specific autoantigens and secreted antibodies. When the team used the same protocol to isolate anti-citrullinated peptide antibodies (ACPA)- and extractable nuclear antigen-reactive autoreactive B lymphocytes from 10 healthy individuals, they were unable to do so. This finding suggests these cells were specific to SLE and RA. However, researchers found no significant relationship between the presence of circulating extractable nuclear antigen- or ACPA-autoreactive B lymphocytes and inflammatory or clinical parameters of either SLE or RA.
Next, the investigators compared the phenotype of extractable nuclear antigen-ACPA-autoreactive B lymphocytes from five individuals with RA and eight individuals with SLE to the total population of CD19+ B cells from these same patients.
“To characterize those autoreactive B lymphocytes, we investigated their phenotype by flow cytometry,” write the authors in their discussion. “Isolated autoreactive B lymphocytes consisted of small, mature CD20+ B lymphocytes. Less than 2% of autoreactive B lymphocytes were CD20-CD27++ cells, thus, likely representing plasmablasts. These results suggest autoreactive B lymphocyte populations incorporate either residual auto-reactive plasmablasts or in vivo activated B cells at an early plasmablast stage.”
The researchers also analyzed the somatic hypermutation of the immunoglobulin heavy chain variable region and found approximately 70% of the clones were not mutated or barely mutated. Additionally, the investigators found IgG anti-extractable nuclear antigen Ab and ACPA production by stimulated extractable nuclear antigen- and ACPA-autoreactive B lymphocytes peaked in the presence of CD40 interactions. This finding suggests autoreactive B cells may be stimulated to differentiate into autoreactive antibody cells.