Typically, nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are the treatments of choice for BCG-related reactive arthritis. Bernini et al found that NSAIDs and corticosteroids were used, alone or in conjunction with other drugs, in 65.1% and 40.4% of cases, respectively.2
Neumayr and colleagues put forth a case report in 2002 on a patient with chronic reactive arthritis related to BCG, and found that the patient had no response to NSAIDs and only a partial response to glucocorticoids. The patient was given isoniazid for three months and had complete resolution of their symptoms. They suggested that, in cases of BCG-related reactive arthritis that do not respond to NSAIDs and glucocorticoids, anti-tuberculosis treatment is indicated.3
In 1986, Lamm et al stated that most of the side effects of BCG could be avoided by giving isoniazid for three days, starting on the first day of BCG treatment.4 Animal models, however, showed a reduction in the immunological effect of BCG when isoniazid was given with it.5 This brings up the obvious question of whether isoniazid decreases the side effects of BCG simply by decreasing BCG’s overall effects via the immune system.
Converse to Neumayr and colleagues, Tinazzi et al recommend immunosuppressive agents, such as methotrexate or cyclophosphamide, if symptoms persist for months to years despite NSAIDs and glucocorticoids.6
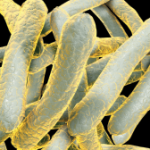
The pathophysiology of reactive arthritis secondary to BCG is unknown, but is believed to occur via a process of molecular mimicry. Animal models have shown that arthritis can develop in a T cell-mediated fashion as a reaction to mycobacterial 65-kD heat shock protein, which was also found to have structural mimicry with a molecule that is cartilage associated and in joints. A similar mechanism may underlie the reactive arthritis seen after BCG administration.7 Other than HLA-B27 positivity, it is unclear what factors put people at risk of developing a chronic form of the arthritis like the one our patient developed.
Back to the Case
Our patient’s presentation is likely chronic reactive arthritis secondary to intravesical BCG given the temporal relationship of his symptoms to BCG administration, as well as the involvement of his low back, sacroiliac joints, knees and ankles, but seronegative RA is another possibility.
Despite the lack of active joint synovitis at the time of our evaluation, the acute onset of sacroiliac joint pain after receiving BCG supports the diagnosis of reactive arthritis. Additionally, his intermittent acute flares of joint pain and swelling also support this diagnosis, and it’s likely he was not in an acute flare at the time we evaluated him.