A fascinating study of five young patients with refractory, active, multi-organ SLE demonstrated improvement in all patients, with four achieving an SLE Disease Activity Index-2K (SLEDAI-2K) of zero by only three months.6 Complement levels normalized and anti-double-stranded DNA antibodies disappeared. All immunomodulatory drugs could be discontinued in all patients, and drug-free remission was maintained at eight months even after reappearance of B cells. “Concerns remain for costs and risks, but this is an innovative approach for which longer follow up in larger numbers will be needed to determine if remission persists,” Dr. Langford concluded.
Dr. Langford briefly touched on litifilimab, a monoclonal antibody that binds blood dendritic cell antigen 2 to suppress the production of type I interferons; iberdomide, an immunomodulatory imide drug that promotes degradation of transcriptional factors Ikaros and Aiolos, reducing B cell activity and type I interferon pathways; and obinutuzumab, a humanized type II anti-CD20 monoclonal antibody that provides greater B cell cytotoxicity and depletion than rituximab. All three therapies were studied in phase 2 randomized trials this year.7-10 “Further studies are needed to better understand the potential roles of these agents, and we look forward to these results in the future,” she said.
Update on COVID-19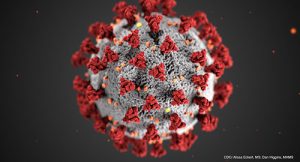
“Throughout this year, we’ve continued to learn about the impact of [COVID-19] on rheumatic disease patients through entities like the Global Rheumatology Alliance, the ACR COVID-19 Task Force and many others,” Dr. Langford said. A systematic literature review demonstrated that patients with rheumatic diseases had a relative risk of developing infection that was 52% higher compared to the general population and a higher risk of poor outcome with a 74% increased risk of death.11 In partially/fully vaccinated patients, another study showed that over half of those requiring hospitalization were receiving a B cell depleting therapy or mycophenolate mofetil.12
Dr. Langford was careful to draw our attention to pre-exposure prophylaxis as a COVID-19 prevention strategy added to non-pharmacologic measures and vaccination. Currently only one agent has received FDA Emergency Use Authorization for pre-exposure prophylaxis (tixagevimab-cilgavimab), but others are likely to follow. This drug doesn’t prevent all COVID-19 infections, but it appears to lessen the frequency and severity with which they occur.13 Dr. Langford encouraged the audience to keep this often-overlooked option in mind for our vulnerable, at-risk immunocompromised patients.
Dr. Langford concluded with an enduring truth: The rheumatology practitioner has played a central role in advocating for immunocompromised patients with rheumatic diseases in the COVID-19 era and will continue to do so. Our evolving roles and contributions as rheumatologists during the changing course of the pandemic are well outlined in a recent Arthritis & Rheumatology publication in August 2022.14

