1. A—Internet-only manuals
Before appealing the request for an overpayment or appealing a denial, providers and staff should first verify the claim was coded and billed correctly. Second, staff should review the internet-only manuals website, which includes operating instructions, policies and procedures that cover CMS policies based on statutes, regulations, guidelines, models and directives. For example, the request for overpayment occurred because an evaluation and management (E/M) visit was billed on the same day as the biologic infusion procedure. According to coding guidelines, unless there is a separate and identifiable reason to bill for an E/M service, then it is not reimbursable. To appeal this, the documentation will need to prove the medical necessity for these two services to be billed together. You can find this rules here, under section 30.6.7.
2. B—Not allowed
The Medicare National Correct Coding Initiative (NCCI), also known as CCI, was implemented to promote national correct coding methodologies and to control improper coding leading to inappropriate payment. The NCCI Procedure-to-Procedure (PTP) code pair edits are automated prepayment edits that prevent improper payment when certain codes are submitted together for Part B-covered services.
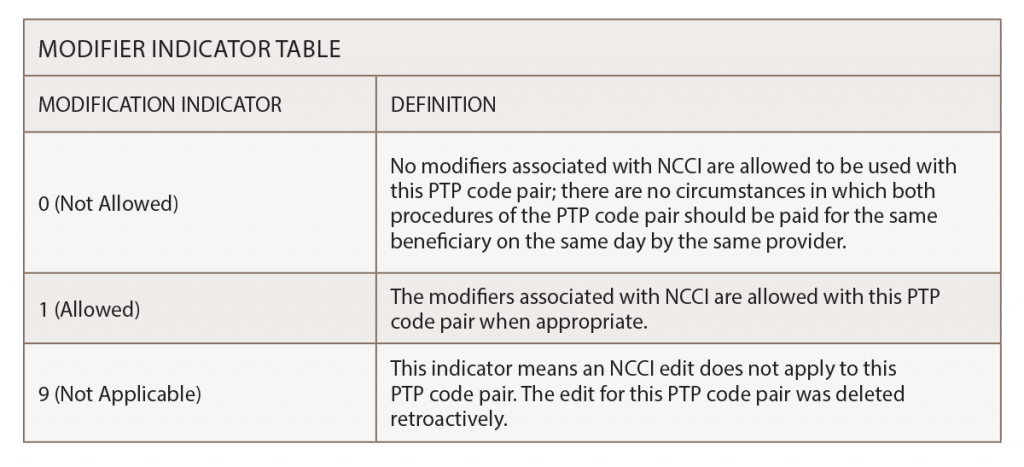
Accurate coding and reporting of services are critical aspects of proper billing. Service denied on the basis of PTP code pair edits or Medically Unlikely Edits may not be billed to Medicare beneficiaries; a provider cannot utilize an Advance Beneficiary Notice of Noncoverage (ABN) to seek payment from a Medicare beneficiary. The NCCI tools found on the CMS website (including the NCCI Policy Manual for Medicare Services) help providers avoid coding and billing errors and subsequent payment denials.
For example, the PTP table lists CPT code 20604 (arthrocentesis, aspiration and/or injection, small joint or bursa [e.g., fingers, toes] with ultrasound guidance), with permanent recording and reporting, and 76942 with an edit modifier “1.” Upon review of the coding columns of the PTP table row for 20604 and 76942, it states that CPT Manual or CMS manual coding instructions indicate CPT code 20604 is inclusive of the guidance—“Ultrasonic guidance for needle placement (e.g., biopsy, aspiration, injection localization device), imaging supervision and interpretation.”
The PTP table can be found here.
3. B—When the table has it listed as “1”
You should not need to do this in all cases, but sometimes it is needed. This can occur when the provider is injecting two joints of the same size, but the injections are not bilateral. For example, the patient needs a joint injection in the right knee and right shoulder; both joints are large but not bilateral. The carrier may reject the claim as a duplicate, but a modifier -59 can be used to bypass this issue.
4. D—All of the above
It is impossible to remove more than one gallbladder on a patient, or to perform a hysterectomy on a male patient. Also, it is against CPT and CMS guidelines to bill 99211-nursing visit with drug administration codes 96360–96415, because the nursing service is built into the relative value unit (RVU) for the drug administration services. The services would be mutually exclusive of one another. RVUs are a measure of value used in the Medicare reimbursement formula for physician services and part of the resource-based relative value scale. The RVU/fee-for-service information can be found here.
5. A—True
All of the medical polices and articles are available on the CMS website and can be filtered by individual states. The list of policies can be found on the CMS website. Once the state is selected, the Local Coverage Determination can be viewed in alphabetical order.
For questions or additional information on coding and documentation guidelines, contact Melesia Tillman, CPC-I, CPC, CRHC, CHA, via email at [email protected] or call 404-633-3777 x820.
