Additional information about his history was obtained. He worked for a pharmaceutical company and as a personal trainer. He denied smoking, illicit drugs, heavy alcohol consumption, or recent travel. His family history was notable for a father with multiple transient ischemic attacks and a maternal uncle with multiple sclerosis (MS). He had no family history of rheumatologic diseases.
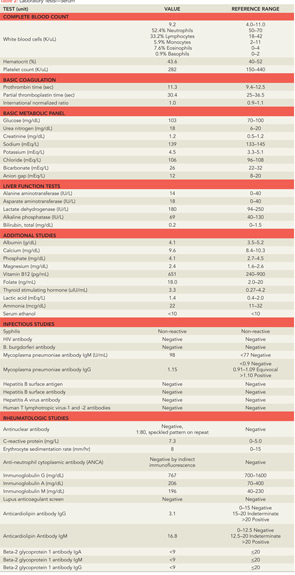
Further laboratory tests were sent (see Table 2). Electroencephalography (EEG) revealed generalized bursts of slowing, consistent with a mild to moderate encephalopathy of toxic, metabolic, or anoxic etiology with no evidence of seizure activity. A repeat MRI of his brain was performed (see Figure 1), which showed innumerable small foci of restricted diffusion scattered over the cerebrum, cerebellum, and brainstem, increased from the prior MRI, with some cortical lesions, but primarily involving the white matter, notably the corpus callosum. The foci were hyperintense on FLAIR imaging and there was persistent leptomeningeal enhancement. There was no evidence of acute infarction or hemorrhage.
Diagnosis
The differential diagnosis at this point was broad. Infectious etiologies were first investigated. Viral etiologies, particularly herpes simplex virus type 1 (HSV-1) encephalitis, characterized by fever, headache, focal neurologic findings, and impaired consciousness, were considered.1 However, SG did not have fevers or a headache, and CSF polymerase chain reaction (PCR), which has very high sensitivity and specificity for detection of HSV-1, was negative.2 Further tests for other infections that can manifest with central nervous system (CNS) involvement, including human immunodeficiency virus (HIV), human T-lymphotropic virus 1 and 2, syphilis, Lyme disease, hepatitis B and C, and tuberculosis, were negative. Toxic ingestions and illicit drugs were also investigated and both his toxicology screen and his serum alcohol level were negative.
Primary neurologic diseases were also considered. Given his initial viral prodrome, the increase in CSF protein, and his MRI findings of multifocal white-matter lesions, post-viral acute disseminated encephalomyelitis (ADEM) was a concern. The possibility of MS was discussed, however his brain MRI findings did not appear to be consistent with this diagnosis, and an MRI of his cervical and thoracic spine showed no evidence of demyelination. Two well-defined gamma-restriction bands were seen in both his CSF and his serum, but this is a nonspecific finding, not suggestive of MS. Creutzfeldt-Jakob disease was considered, given his memory loss and psychiatric symptoms; however, he had no evidence of myoclonus, and did not exhibit rapid mental deterioration.3 Malignancy, especially lymphoma, was plausible given the leptomeningeal enhancement seen on his MRI; CSF cytology, however, was negative for malignant cells.