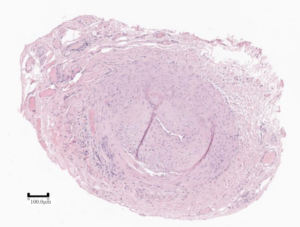
Figure 1: Active arteritis. Inflammatory cells are present in the media in the lower left aspect of the vessel wall. (Click to enlarge.)
At the end of 2023, the Society for Cardiovascular Pathology (SCVP) published consensus guidelines on the diagnostic approach to temporal artery biopsy.1 Through this publication, SCVP hopes to bring more uniformity to the processing, interpretation and reporting of these specimens, taking into consideration the most up-to-date literature available. These guidelines have obvious impact on clinical practice, particularly in the diagnosis and, thus, management of giant cell arteritis (GCA). We wish to highlight some of the important messages from our consensus document and engage the rheumatology community in synthesizing such guidelines into future, unified diagnostic criteria.
Gold Standard for GCA Diagnosis
Although imaging criteria continue to improve, the current standard against which the sensitivity and specificity of those studies is measured is biopsyproven disease. The 2021 ACR/Vasculitis Foundation Guideline speaks to recommendations specifically for the use of biopsy in diagnosing GCA, although it acknowledges the recommendations are conditional and with low level of evidence.2
We acknowledge the broader, and reasonable, recommendations in the 2022 ACR/EULAR classification criteria.3 Nonetheless, we (admittedly somewhat self-servingly) support the recommendation of continuing to use biopsy as a gold standard at a minimum until higher quality evidence for other diagnostic techniques or algorithms is available.
The imperfect sensitivity of temporal arterial biopsy for GCA (currently estimated at 61–77%), given the spatial and temporal heterogeneity of the disease, however, is acknowledged.4,5 In cases of high clinical suspicion and negative biopsy, we obviously support the utility of imaging and other diagnostic modalities.
Healed Injury Is Not Specific for Arteritis
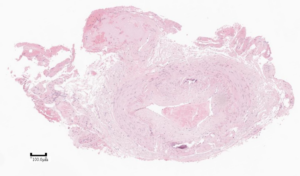
Figure 2: Healed arterial injury. There is intimal hyperplasia, adventitial fibrosis, and calcification of the internal elastic lamina (Monckeberg’s medial calcification), but no inflammation. (Click to enlarge.)
“Healed arteritis” has received much attention in the literature over the years, with a number of criteria proposed, but without certainty as to the clinical significance. The latest evidence available to us at the time we wrote our guidelines, however, demonstrates that all the findings of healed arteritis can be seen in cases without GCA or any other vasculitis.
Histomorphologically, there is overlap between trauma (accidental, iatrogenic, prior biopsy), age-related changes and healed arteritis. Hence we specifically recommend the diagnostic term “healed arterial injury” to reflect that something damaged the temporal artery, but we cannot comment as to the etiology. This is an important recognition in developing future diagnostic algorithms because the degree to which post-test probability is informed by “healed arteritis” is insufficiently studied.


