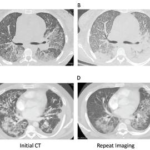
A variety of immune and nonimmune pathophysiologic mechanisms causing the disruption of alveolar capillaries with bleeding into the alveolar spaces can lead to diffuse alveolar hemorrhage (DAH). Immune-mediated mechanisms can cause DAH with or without the presence of capillaritis. The antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV) syndromes—granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA)—are the most common cause of pulmonary capillaritis leading to DAH. DAH is a severe manifestation of AAV, commonly associated with glomerulonephritis and often leading to respiratory failure requiring ventilatory support in the intensive care unit (ICU).
Customary therapy for AAV-related DAH has consisted of remission induction with high-dose pulse methylprednisolone followed by daily oral glucocorticoids in combination with cyclophosphamide. More recently, rituximab has been introduced as an alternative to cyclophosphamide. For patients with respiratory failure and severe renal disease, plasma exchange (PE) has been advocated as an adjunct, even though its therapeutic efficacy is not well supported by the literature.
These researchers set out to identify factors that predict respiratory failure and to evaluate the therapeutic efficacy of plasma exchange and of rituximab vs. cyclophosphamide in a cohort of patients with DAH secondary to AAV with or without respiratory failure.
They performed a single-center historical cohort study of all consecutive patients with AAV-associated DAH who were evaluated over a 16-year period. Logistic regression models were developed to examine the predictive role of the baseline clinical characteristics for the development of respiratory failure, and for the effect of PE and remission-induction therapy on the main outcome (complete remission at six months).
Seventy-three patients with DAH were identified, and 34 of them experienced respiratory failure. The degree of hypoxemia upon initial presentation, a higher percentage of neutrophils in the bronchoalveolar lavage fluid cell count, and higher C-reactive protein levels were independently associated with the development of respiratory failure. PE was not associated with achieving complete remission at six months, with an odds ratio (OR) of 0.49 (95% confidence interval [95% CI] 0.12–1.95) (P50.32). Rituximab treatment was independently associated with achieving complete remission at six months (OR 6.45 [95% CI 1.78–29], P 5 0.003).
The researchers found the most important predictor of respiratory failure in patients with DAH secondary to AAV is the degree of hypoxemia upon presentation. No clear benefit of the addition of PE to standard remission induction therapy was demonstrated. Complete remission by six months was achieved at a higher rate with rituximab than with cyclophosphamide. Because remission by six months was achieved at a higher rate with rituximab than with cyclophosphamide in patients with DAH secondary to AAV, including those who need mechanical ventilation, rituximab may be preferable for this subset of patients.
Excerpted and adapted from:
Cartin-Ceba R, Diaz-Caballero L, Al-Qadi MO, et al. Diffuse alveolar hemorrhage secondary to antineutrophil cytoplasmic antibody–associated vasculitis: Predictors of respiratory failure and clinical outcomes. Arthritis Rheumatol. 2016 Jun;68(6):1467–1476.