CHICAGO—In systemic lupus erythematosus (SLE), most types of severe pulmonary manifestations are relatively rare, but it’s crucial they be caught because of the potentially dire consequences, said Richard Silver, MD, professor in the Rheumatology Division at the Medical University of South Carolina, Charleston, at the 2018 ACR/ARHP Annual Meeting.
Pulmonary Manifestations
Parenchymal disease—seen in the form of acute lupus pneumonitis, acute respiratory distress syndrome, diffuse alveolar hemorrhage and chronic interstitial pneumonitis—appears in less than 5% of lupus patients. Its mortality rate can run as high as 50%.
“When you see it, you’ve got to recognize it. You’ve got to know you’ve seen it because it can be catastrophic,” Dr. Silver said.
Acute lupus pneumonitis (ALP) usually presents with abrupt fever onset, cough, pleurisy and dyspnea, and is marked by evidence of lupus activity, such as double-stranded DNA antibodies, low C3 and C4, pleural effusions and alveolar infiltrates. The initial concern should be excluding infection, with immunosuppression treatment once infection is ruled out.
Diffuse alveolar hemorrhage (DAH), also rare but potentially fatal, can resemble ALP, but if hemoptysis is also present, consider DAH, Dr. Silver said. A falling hematocrit is a telltale sign of DAH, and rituximab has shown efficacy in its treatment.1
Risk factors for pulmonary arterial hypertension (PAH) in SLE include Raynaud’s phenomenon, anti-U1 RNP antibodies, anti-cardiolipin antibodies and anti-endothelial cell antibodies. High-risk patients can be screened with pulmonary function tests and echocardiogram, though the gold diagnostic standard is right heart catheterization.
A diagnosis occurs when a high pulmonary arterial pressure with a non-elevated pulmonary capillary wedge pressure and a pulmonary vascular resistance of greater than or equal to 3 Wood units are evident.
“You might have pulmonary hypertension on an echo or even on a right heart catheterization,” Dr. Silver said, “but if the [wedge pressure is elevated], it’s not PAH. It’s diastolic dysfunction or some other cardiac issue leading to pulmonary hypertension. Unless it’s PAH, you shouldn’t embark on PAH-specific therapy.”
More therapeutic options have emerged in recent years, he said.
“We now have a host of PAH-specific therapies,” Dr. Silver said. “Most people would either use monotherapy with an oral agent, or a dual combination oral therapy using both a PDE5 inhibitor and an endothelin receptor antagonist (ERA). This really requires the input of a PAH specialist. If patients are failing mono- or dual-combination therapy, that therapy needs to be escalated, and this usually requires a multidisciplinary approach.”
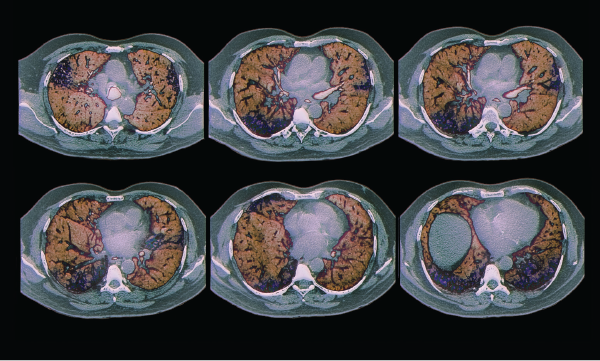
Colored computed tomography (CT) scans of axial sections through the chest of a 68-year-old patient with interstitial lung disease (diffuse parenchymal lung disease, DPLD). Parenchymal disease appears in less than 5% of lupus patients.
Zephyr / Science Source
Kidney Manifestations
Severe lupus manifestations in the kidney can prove challenging to manage, said Derek Fine, MD, a nephrologist and associate professor of medicine at Johns Hopkins, Baltimore. But he offered these suggestions on how to make the best of a challenging situation:
- First, make sure the patient is actually taking their medications properly. “If you really drill down, many of our resistant patients actually are not taking their medications, either appropriately or at all. And it’s just a matter of having them admit to that.”
- Response matters. Those who don’t respond end up doing “very, very, very poorly,” with high rates of dialysis at 10 years, Dr. Fine said. Those with a good response do well. An “unacceptable” number of patients among the intermediate-responders end up on dialysis with end-stage renal disease. He said, “Our goal is to really get everyone into complete remission.”
- When to biopsy a patient is the only portion of the ACR guidelines on induction therapy with which he disagrees. The guidelines recommend a biopsy for patients with 1 g of proteinuria, but Dr. Fine prefers a lower threshold. “My level is 500 mg,” he said. “I believe strongly more than 500 mg of proteinuria would be an indication for kidney biopsy.”
- Many good reasons exist to obtain a kidney biopsy, such as to detect class switching, assess lesion severity and catch other diagnoses. Biopsy can also help identify class altering, which can bring important therapeutic considerations. About a third of patients at his center are a combined proliferative with membranous lupus. And this status could change with treatment. “If you’re treating and they’re not getting better, what’s left behind?” he said. “Frequently, I find the proliferative component disappears and the membranous component remains. … I don’t necessarily need to change their therapies. So it makes a huge difference.”
- Multi-target therapy with mycophenolate mofetil (MMF) plus the calcineurin inhibitor tacrolimus have been shown to work better than cyclophosphamide in induction. It has not been rigorously studied in the refractory setting, but it is an option for these patients, he said.2
- The word crescents should set off alarm bells. “When you hear the word crescent, think bad, even if it’s one,” Dr. Fine said. “The pathologists will say, ‘One out of 20 glomeruli have crescents.’ Well, you have 2 million nephrons. That means you have 100,000 nephrons at risk of loss at that point.”
- Rituximab data are not impressive in treatment of lupus nephritis. But a review of reported uses found a complete response in 40% of cases and a partial response in 34% of cases.3 “It’s better than nothing,” Dr. Fine said, adding the results for rituximab suffer from a publication bias, with only positive results seeing the light of day. Still, it’s a “reasonable” option, he said.
- Voclosporin, a treatment still being explored, is a modified cyclosporine with a more predictable pharmacokinetic/pharmacodynamic relationship, making it more tolerable. Results in 265 patients showed significant rates of complete remission, although the data included 13 deaths, which investigators did not attribute to the medication. Clinicians “have to [exercise] some caution” with the treatment, Dr. Fine said.4
- Combining rituximab with belimumab is being explored to address the problem of autoreactive plasmoblasts proliferating in rituximab non-responders, due to high B cell activating factor (BAFF) levels. The idea is to chase rituximab with anti-BAFF belimumab to knock down this BAFF escalation, Dr. Fine said, and it has produced reasonable responses. “I think we need to see more data,” he said.
Thomas R. Collins is a freelance writer living in South Florida.
References
- Tse JR, Schwab KE, McMahon M, et al. Rituximab: An emerging treatment for recurrent diffuse alveolar hemorrhage in systemic lupus erythematosus. Lupus. 2015 Jun;24(7):756–759.
- Liu Z, Zhang H, Liu Z, et al. Multitarget therapy for induction treatment of lupus nephritis: A randomized trial. Ann Intern Med. 2015 Jan 6;162(1):18–26.
- Weidenbusch M, Römmele C, Schrottle A, et al. Beyond the LUNAR trial. Efficacy of rituximab in refractory lupus nephritis. Nephrol Dial Transplant. 2013 Jan;28(1):106–111.
- Tumlin JA, Rovin B, Rahman MM, et al. Steroid sparing efficacy of voclosporin in active lupus nephritis: Stable kidney function and blood pressure without electrolyte complications at 48 weeks. Presented at European Renal Association-European Dialysis and Transplant Association Congress. 2017 Jun. Madrid.

