Discussion
HLH is broadly divided into two categories: primary HLH, which typically occurs in infants and children, and secondary HLH, which occurs in adults.1 HLH is characterized by an uncontrolled immune response, leading to tissue infiltration by natural killer (NK) cells, cytotoxic T cells and macrophages, and by the release of proinflammatory cytokines, including tumor necrosis factor alpha (TNFα), IL-1 and IL-6, which lead to tissue damage.1
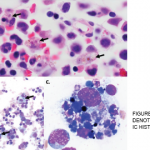
Activated macrophages accumulate in the tissues, including bone marrow, lymph nodes, liver and spleen, which leads to phagocytosis of normal cells—the pathognomonic feature of HLH seen in tissue biopsy.
Primary HLH, including familial HLH (autosomal recessive mutations) and lymphoproliferative syndromes, is caused by genetic mutations impairing the function of NK and T cells. Secondary HLH is usually triggered by an underlying condition, and it may have been related to AAV in our patient.2
Predisposing conditions that have been reported include viral infections (most commonly Epstein-Barr virus), malignancies (leukemias and lymphomas) and rheumatologic illness.
Specific diagnostic criteria for adult-onset HLH are not well established. The diagnosis in adults is based on application of the 2004 pediatric diagnostic criteria (see Table 3, below).4,5 Other clinical and laboratory findings that are supportive of HLH diagnosis in adult population (but are not part of the pediatric diagnostic criteria) include hepatomegaly, transaminitis, elevated LDH, elevated D-dimer with normal INR and PTT, coagulopathy, elevated CRP, hyponatremia, rash and neurologic involvement.2 Genetic mutations are part of the diagnostic criteria, but are not routinely tested in adults.
| DIAGNOSTIC CRITERIA FOR HLH | ||
|---|---|---|
| Molecular tests | ||
| Genetic mutation | PRF1 | |
| UNC13D | ||
| TX11 | ||
| STXBP2 | ||
| RAB27 | ||
| XLP | ||
| Or | ||
| 5 of 8 clinical criteria | Fever | Peak temperature of >38.5°C |
| for >7 days | ||
| Splenomegaly | Spleen palpable >3 cm below costal margin | |
| Cytopenias of at least two lineages in the peripheral blood | Hemoglobin <9 g/100 mL | |
| Platelets <100 X 103/mL | ||
| Neutrophils <1 X 103/mL | ||
| Hypertriglyceridemia | Fasting, ≥265 mg/100 mL | |
| and/or hypofibrinogenemia (≤150 mg/100 mL) | ||
| Hemophagocytosis in bone marrow (BM), spleen or lymph nodes | Low or absent NK cell activity | |
| Ferritin ≥500 ng/mL | ||
| Low or absent natural killer cell activity | ||
| Soluble CD25 (that is, soluble IL-2 receptor) >2,400 U/mL | ||
| PRF1: Perforin protein; UNC13D: Munc 13-4 protein; STX11: Syntaxin 11 protein; STXBP2: Munc 18-2 protein. |
Early in the disease process, HLH can be overlooked, especially given the nonspecific nature of the symptoms and its association with other conditions. Clinical findings of HLH are similar to those of systemic inflammatory response syndrome (SIRS) and are often initially treated as an infection, as in this case. Hyperferritenemia with values >10,000 ng/mL is 90% sensitive and specific in the pediatric population. In adults, however, hyperferritenemia is less specific. In fact, levels as high as 50,000 ng/mL have been reported in infections, hepatocellular injury, renal failure and other conditions.6
Relative changes in overall clinical and laboratory parameters is a good way to make an early diagnosis of MAS.9 In our patient’s case, there was a drop in ESR and a discordance between ESR and CRP levels. This discordance is often found in early cases of MAS.9
Although pathognomonic, hemophagocytosis is neither sensitive nor specific for HLH.1 Hemophagocytosis may not be seen in a bone marrow aspiration or biopsy in early stages of HLH. Sometimes, even when not seen on bone marrow examination, autopsy examination of the spleen or lymph nodes may reveal hemophagocytosis. Bone marrow biopsy should be performed when considering a diagnosis of HLH, not only for diagnosis but also to exclude hematological malignancy as the trigger.1,6,7 Repeating it may also be necessary in later disease stages.
Soluble IL-2 receptor CD 25 has recently been reported as a low-cost diagnostic test for HLH in adults. Along with ferritin and lactate dehydrogenase (LDH), the IL-2 receptor assay is a useful way to assess treatment response. However, IL-2 receptor testing is mostly performed in reference laboratories, and it may take several days to obtain results.1,2