
Image Credit: Lightspring/shutterstock.com
In diagnosing and treating a disease that is rapidly gaining recognition worldwide since it was first recognized in Japan in 2003, 42 experts from 10 different countries recently collaborated to discuss and review the current experience and data on IgG4-related disease.
The result is the “International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease,” published in July 2015 in Arthritis & Rheumatology.1
A Systemic Disorder
Defined as a fibroinflammatory condition mediated by the immune system that can affect multiple organs and lead to tumefactive, tissue-destruction lesions and organ failure, IgG4-related disease is now recognized as a systemic disorder that links many individual organ conditions once thought not to be related.1
Diagnosis is complicated by the many conditions that can mimic the disease. The disease is often mistaken for a malignancy, an infection or other immune-mediated conditions, such as Sjögren’s syndrome, giant cell arteritis or granulomatosis with polyangiitis.
“IgG4-related disease is an emerging systemic condition linking many disorders once regarded as isolated, single-organ conditions that were managed by different subspecialties,” says Arezou Khosroshahi, MD, assistant professor of medicine, Rheumatology Division, Emory University School of Medicine, Atlanta, and lead author of the study. “Most patients with IgG4-related disease undergo multiple invasive procedures for suspected malignancy before the diagnosis is considered, which delays their diagnosis and on-time treatment.”
According to Dr. Khosroshahi, the disease has only been recognized in the U.S. in the past decade and published evidence on the disease is still quite thin, with no prospective, randomized trials yet available.
Given the rapid recognition of the disease within the past decade, however, experts felt some guidance was needed to help clinicians diagnose and manage a complicated disease that can affect multiple organs, most commonly the pancreas, biliary tract, major salivary glands, lacrimal glands, retroperitoneum and lymph nodes. Indeed, because of the widespread anatomical areas in which the disease can present, experts representing eight specialties (i.e., gastroenterology, rheumatology, ophthalmology, pulmonary-critical care, hematology/oncology, internal medicine, nephrology and endocrinology) were among the experts included in the development of the consensus statement.
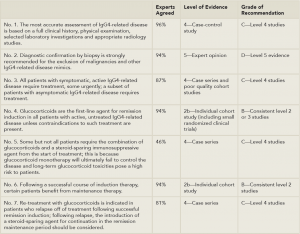
(Click for larger image)
Table 1: 7 Key Consensus Statements
Adapted and compiled from References 1 and 2.
The consensus statement offers clinicians seven key statements to help guide diagnosis and treatment of IgG4-related disease (see Table 1). The primary evidence available and used to base these statements on came primarily from individual small cohorts, case series and expert opinions in the literature, according to Dr. Khosroshahi. Each statement is accompanied by the percentage of experts who agreed with the statement, along with the quality of evidence based on the Oxford Centre for Evidence-Based Medicine (OCEBM), in which the level of evidence is graded from 1a-5 (1a being the best quality of evidence) and grade of recommendation ranges from A (strongest recommendation) to D (lowest).2 (For more information on the OCEBM grading system.)
“The goal of creating this International Consensus Guidelines Statement was to capture the expertise of clinicians and clinical investigators from across the world with extensive experience in the management and treatment of IgG4,” says Dr. Khosroshahi, adding that the guidelines are intended to help inform clinical management of this disease worldwide until better cohort and prospective studies are conducted.
Takeaway for Rheumatologists
One key message highlighted by the findings of the consensus statement is the importance of accurate and early diagnosis to ensure optimal management of the disease that can affect many organs.
The senior author of the study, John H. Stone, MD, MPH, professor of medicine, Harvard Medical School, director of clinical rheumatology, Massachusetts General Hospital, Boston, emphasized that the guidance statement indicates for the first time that experts agree on a low threshold for initiating treatment in patients with active disease. As shown in Table 1, recommendation No. 3, 87% of experts agreed on the importance of early treatment.
“Although IgG4-related disease generally has a subacute presentation, irreversible injury to some organs can occur within weeks or months if effective therapy is not initiated,” he says, emphasizing that a major goal of therapy identified by the experts is the prevention of fibrosis.
“Once fibrosis is established, therapeutic options are currently limited,” Dr. Stone says.
Clinical manifestations that require urgent therapy, he says, include aortitis, retroperitoneal fibrosis, proximal biliary strictures, tubulointerstitial nephritis, pachymeningitis, type 1 autoimmune pancreatitis and pericarditis.
Commenting on the consensus statement, Eric Matteson, MD, chair of the Division of Rheumatology, Mayo Clinic, Rochester, Minn., highlighted the help offered by the consensus statement in underscoring the numerous conditions associated with IgG4-related disease, as well as the conditions that mimic this disease.
One key message … is the importance of accurate & early diagnosis to ensure optimal management of the disease that can affect many organs …. [I]rreversible injury to some organs can occur within weeks or months if effective therapy is not initiated.
He also stresses the importance of prompt treatment. “The guidelines help emphasize the need for recognition of, and prompt and aggressive treatment of the disease, which substantially limit the organ damage and comorbidities associated with it,” he says.
To help make the diagnosis, Dr. Stone emphasizes the need for close collaboration between clinicians and pathologists because neither clinical nor pathologic findings alone are sufficient for diagnosis in most cases.
“I find it enormously helpful to sit at the microscope with the pathologist and review biopsy slides myself,” he says, adding that the collaboration is equally beneficial to the pathologist and generates a “remarkable synergy.”
“We call this ‘clinicopathologic correlation,’ and there is no disease for which it is more important than IgG4-related disease,” he says.
Dr. Stone also emphasizes that this clinicopathologic correlation, along with histologic features, are more important to establishing a diagnosis than the use of serum IgG4 concentrations, which, he says, are important, but need to be better understood.
Use of Glucocorticoids
One area of particular emphasis, according to Dr. Stone, is the use of glucocorticoids. Even though strong consensus was reached by the experts on the effectiveness of these agents as initial therapy for most patients, Dr. Stone emphasizes that glucocorticoids are often tolerated poorly, and disease recurrences are common during or after tapering off these agents.
“Our extensive experience with glucocorticoids in IgG4-related disease makes us keenly aware of the frequency with which these agents fail in IgG4-related disease and the high morbidity that can result if they are used inappropriately,” he says.
He also emphasizes that few data support the effectiveness of conventional steroid-sparing agents to treat IgG4-related disease.
Rather, Dr. Stone suspects that future treatment of IgG4-related disease will involve biologic therapies that he believes will “lead to dramatic improvements in clinical outcomes.”
Mary Beth Nierengarten is a freelance medical journalist based in St. Paul, Minn.
References
- Khosroshahi A, Wallace ZS, Crowe JL, et al. International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease. Arthritis Rheumatol. 2015 Jul;67(7):1688–1699.
- Oxford Centre for Evidence-Based Medicine. 2009 March.


