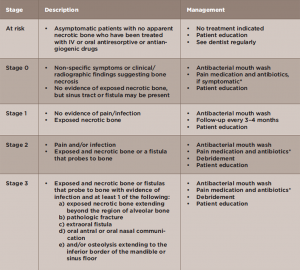
Management of MRONJ depends on disease stage (see Table 1).5 The aims of treatment are to prevent infection and pain in asymptomatic

Figures 4A & B: Nonsurgical sequestrectomy: (top) necrotic bone on lingual mandible; and (bottom) removal of fragment of necrotic bone by simple mobilization.
Stage 1 cases, to control pain and infection in Stage 2 cases and to mobilize and remove sequestra in all cases. Stage 3 cases may require surgery and, within the past few years, surgery has been used increasingly and successfully to manage even Stage 2 cases.58
Regardless of the stage, an attempt should be made to gently dislodge the bone fragment (nonsurgical sequestrectomy) at each visit (see Figures 4A–B, left). All patients are placed on an anti-microbial mouth rinse, such as chlorhexidine digluconate. Other treatment modalities include hyperbaric oxygen, laser therapy, ozone therapy, autologous platelet-rich plasma (e.g., VEGF, PDGF, TGF-ß) or teriparatide, although no controlled studies are available for these treatment modalities.59
Adverse effects associated with the use of bisphosphonates include gastrointestinal upset, acute-phase reactions, & renal toxicity.
Studies have investigated bone turnover markers (e.g., C-terminal crosslinked telopeptide [CTx]) both in serum and saliva to assess the risk of developing MRONJ in patients taking bisphosphonates with some promising, but not definitive results.60 Although low serum CTx was considered to be an important marker for bisphosphonate-associated osteonecrosis, this is not specific because after all, low bone turnover markers are an expected and desired outcome in patients given anti-resorptive agents.
Subsequent studies have confirmed the unreliability of this marker for prediction of disease. Although the use of such markers for MRONJ risk is not recommended by the AAOMS, research on this topic merits attention.61,62
Conclusions
There has been much active, ongoing research in the field of MRONJ over the past 12 years since MRONJ was widely recognized, and this has helped us better understand the etiopathogenesis, genetic predisposition, risk assessment, diagnosis of early lesions and management of MRONJ. By working closely together, dentists and physicians can help minimize the occurrence of this condition and treat patients expeditiously if they develop it.
Alessandro Villa, DDS, PhD, MPH, is an associate surgeon in the Division of Oral Medicine and Dentistry, Brigham and Women’s Hospital, and an instructor in the Department of Oral Medicine, Infection and Immunity, Harvard School of Dental Medicine, Boston.