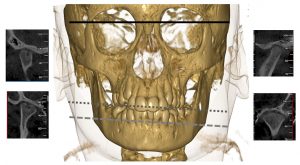
A cone beam CT of an 11-year-old boy with arthritis in the right temporomandibular joint (TMJ). The right TMJ displays deformity with flattening of the condylar head and tuberculum, cortical erosion and a cyst. The left temporomandibular joint has a normal radiographic appearance. There is a notable mandibular asymmetry canting toward the right because of arthritis-induced reduction in facial growth and development in this side (gray reference lines).
Juvenile idiopathic arthritis (JIA) can affect all joints, including the temporomandibular joints (TMJs). For a long time, the TMJ was a “forgotten” joint in pediatric rheumatology, although Sir Frederick Still did comment on a small mandible in his first case series on juvenile arthritis in 1897. In recent years, more attention has been given to the TMJ in JIA; however, the joint is still grossly overlooked in clinical trials and treatment studies due to its difficult-to-assess nature. Orofacial clinical examination recommendations were published in 2017, which will, hopefully, lead to better assessment of this joint in clinical trials and treatment studies.1
The TMJ is a unique joint due to developmental, anatomic and histological properties. In addition, the TMJs perform complex functional movements; the two joints function as one joint during mouth opening. Each TMJ consists of the condyle and the fossa, with an interposed articular disc. The mandibular growth plate is positioned directly underneath the articular surface of the condyle.
Physical damage, such as direct compression or TMJ inflammation, can cause severe mandibular growth disturbances. In patients with JIA, unilateral TMJ involvement can lead to facial asymmetry, and bilateral involvement can lead to retrognathia, the so-called bird-face appearance. Any change in mandibular growth can lead to orofacial signs and symptoms, changes in bite, and therefore, functional and esthetic problems.
In short, TMJ arthritis relates to more than just the jaw joint itself. Signs and symptoms can persist into adulthood and may have a significant impact on general quality of life.2-4
Diagnosis & Challenges
Most patients with JIA-associated TMJ arthritis don’t display symptoms or report any complaints until symptoms cause functional problems and potential damage has occurred. Without consistent, standardized clinical evaluation, the only way to establish the presence of TMJ inflammation is by imaging.
Terminology surrounding JIA-associated TMJ arthritis has been conflicting in the past, making it difficult to compare studies. To enhance collaboration, consensus-based terminology for JIA-related orofacial manifestations were proposed by the Temporomandibular Joint Juvenile Arthritis Working Group (TMJaw; formerly known as euroTMjoint).5 The TMJaw is an international, interdisciplinary network of specialists with a special interest in research and management of TMJ arthritis in JIA.
TMJaw has defined TMJ arthritis as “active inflammation in the TMJ.” TMJ arthritis can be assessed only by gadolinium-enhanced magnetic resonance imaging (MRI) to view the active component of synovial fluid and tissue enhancement. In the absence of signs of active TMJ arthritis on MRI, patients may still have TMJ involvement, defined as “clinical and/or radiological abnormalities presumed to be the result of previous TMJ arthritis.”4
Other imaging techniques used to display the TMJ, such as ConeBeam computed tomography (CT), ultrasound, orthopantomogram or lateral cephalographs, cannot provide answers regarding TMJ arthritis.
TMJ arthritis can present in any patient with JIA, and the TMJ can be involved at any time of the disease course. Occasionally, the TMJ may be the only joint involved.6
Difficulty remains in knowing how to efficiently diagnose and monitor TMJ arthritis. Many clinicians perform an MRI at disease onset, and if it’s normal repeat the MRI if the patient reports any symptoms or there are relevant findings during clinical examination.
MRI evaluation needs to be performed by a radiologist aware of the normal appearance of the joint during the course of the child’s development. Kellenberger et al. have developed a pictorial atlas depicting the TMJ’s normal and abnormal appearance for different ages.7 If the MRI shows TMJ arthritis and treatment is started, clinicians can repeat the MRI three to six months later, depending on expected treatment effect.
No studies have been performed to determine the perfect follow-up period for the MRI. The patient’s age and need for sedation, costs and clinical consequences have to be taken into account. More research on less invasive diagnostic tests is necessary to be able to continuously evaluate this joint.
Another dilemma: Arthritis-induced orofacial signs and symptoms may persist in patients without current MRI findings of TMJ inflammation. Also, dentofacial deformity may progress in well-treated patients. A clinical orofacial examination is an important aspect of the full-body examination of JIA patients. The TMJaw group has published clinical orofacial examination recommendations for monitoring patients in clinical practice and research studies to ensure the TMJ is examined during every clinical visit with a JIA patient.1 These recommendations include obtaining a complete medical history and assessing for the presence of orofacial symptoms. The clinical examination should include palpation of the TMJ and masticatory muscles. The orofacial function evaluation should include assessment of TMJ function (maximal mouth opening and movement) and assessment of facial morphology and symmetry.1
Treatment
Treatment goals for JIA-associated TMJ arthritis are to prevent progression of condylar damage and dentofacial deformity; decrease orofacial symptoms, such as pain; and prevent progression or reverse orofacial dysfunction.
Management of TMJ arthritis should be led by a multidisciplinary team, including but not limited to a pediatric rheumatologist, physiotherapist, orthodontist, oral maxillofacial surgeon, radiologist and dental specialist. The team’s composition depends on location and the patient’s healthcare system.
Treatment can roughly be divided into four different categories: 1) reducing TMJ inflammation (i.e., systemic and intra-articular treatment); 2) controlling signs and symptoms via oral splints, physiotherapy, adjustment to systemic treatment or arthrocentesis; 3) normalizing mandibular growth (via oral splints); and 4) surgical correction of TMJ/dentofacial deformity in skeletally mature patients.

These clinical photographs depict an acrylic distraction splint worn full time. Every six to eight weeks, a thin layer of acrylic is added to the right sight of the splint to distract this side of the face and normalize mandibular growth and development.
Disease-modifying anti-rheumatic drugs (DMARDs) and biologics are also used for the treatment of JIA-associated TMJ arthritis. The exact effect of these treatments remains unanswered in studies with TMJ MRIs pre- and post-treatment. However, empirical practice suggests these treatments are as effective for the TMJ as for other peripheral joints. Earlier initiation of treatment is believed to give better outcomes than treatment late in the TMJ arthritis course. A recent Swiss study showed improvement of the TMJs on systemic treatment.8
Intra-articular corticosteroid injections (IACs) were routinely used for TMJ arthritis, as for other peripheral joints in JIA. However, studies have shown a reduced growth of the mandible after TMJ IACs in animals, and these findings have been supported by retrospective human data, suggesting that treatment of TMJ arthritis with IACs can lead to reduced mandibular growth.9,10 The current recommendation is not to use IACS for the management of TMJ arthritis—and certainly not repeated IACs—in skeletally immature JIA patients. Intra-articular heterotopic bone formations have also been associated with IACs, especially if use is recurrent throughout the disease course.
IACs can be used to treat TMJ arthritis in skeletally mature individuals.
Orthopedic devices, such as oral splints, have proved effective for the treatment of orofacial symptoms associated with TMJ arthritis and in the reduction of dentofacial deformities from TMJ arthritis in growing individuals.11,12 Orthopedic devices are routinely used in Scandinavian countries for the treatment of JIA-associated TMJ involvement; however, such devices may be difficult to obtain in other healthcare systems in other countries due to their cost. Orthodontic treatment of JIA-associated dentofacial deformity requires special training, and availability of this treatment is, for now, limited.
Maxillofacial surgery is often a last resource for severely affected patients for either functional or esthetic reasons. In the biologic era, the need for orthognathic surgery or joint replacement has decreased, and severe growth impairment, such as the bird-face appearance, is rarely seen. Maxillofacial surgical options include orthognathic surgery, distraction osteogenesis and TMJ reconstruction—autogenous or alloplastic. The TMJaw surgical group has developed surgical recommendations for JIA-associated TMJ arthritis describing the timing for the different options.13
Conclusion
JIA-associated TMJ arthritis occurs frequently and can have a devastating impact on TMJ function and facial growth and development.
Diagnosis is complicated by the need for a gadolinium-enhanced MRI to confirm the presence of active arthritis and to steer the right treatment. Facial signs and symptoms and dentofacial deformity may progress in well-treated patients.
Patients with TMJ arthritis should receive systemic treatment, and skeletally mature patients should receive intra-articular corticosteroid injections. Symptoms due to TMJ involvement, including TMJ dysfunction, can be treated with orthopedic devices, physiotherapy and, in extreme cases, with surgical intervention. Outcomes improve with early diagnosis and initiation of treatment.
To improve the oral, maxillofacial, health-related quality of life of our JIA patients, rheumatologists need to be aware of the potential involvement of the TMJs in JIA. Monitoring the TMJs during each clinic visit through a standardized clinical examination is necessary.
Marinka Twilt, MD, MSCE, PhD, is an assistant professor of pediatrics at the Cumming School of Medicine, University of Calgary, Alberta, Canada, and a pediatric rheumatologist at the Alberta Children’s Hospital, Calgary.
Peter B. Stoustrup, DDS, PhD, is an associate professor of orthodontics in the Section of Orthodontics, Aarhus University, Denmark.
References
- Stoustrup P, Twilt M, Spiegel L, et al. Clinical orofacial examination in juvenile idiopathic arthritis: International consensus-based recommendations for monitoring patients in clinical practice and research studies. J Rheumatol. 2017 15 Mar;44(3):326–333.
- Stoustrup P, Glerup M, Bilgrau AE, et al. Cumulative incidence of orofacial manifestations in early juvenile idiopathic arthritis: A regional, three-year cohort study. Arthritis Care Res (Hoboken). 2019 Apr 11. [Epub ahead of print]. doi: 10.1002/acr.23899
- Frid P, Nordal E, Bovis F, et al. Temporomandibular joint involvement in association with quality of life, disability, and high disease activity in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2017 May;69(5):677–686.
- Rahimi H, Twilt M, Herlin T, et al. Orofacial symptoms and oral health-related quality of life in juvenile idiopathic arthritis: A two-year prospective observational study. Pediatr Rheumatol Online J. 2018 Jul 13;16 (1):47.
- Stoustrup P, Resnick CM, Pedersen TK, et al. Standardizing terminology and assessment for orofacial conditions in juvenile idiopathic arthritis: International, multidisciplinary consensus-based recommendations. J Rheumatol. 2019 May;46(5):518–522.
- Hügle B, Spiegel L, Hotte J, et al. Isolated arthritis of the temporormandibular joint as the initial manifestation of juvenile idiopathic arthritis. J Rheumatol. 2017 Nov;44(11):1632–1635.
- Kellenberger CJ, Junhasavasdikul T, Tolend M, Doria AS. Temporomandibular joint atlas for detection and grading of juvenile idiopathic arthritis involvement by magnetic resonance imaging. Pediatr Radiol. 2018 Mar;48(3):411–426
- Bollhalder A, Patcas R, Eichenberger M, et al. Magnetic resonance imaging followup of temporomandibular joint inflammation, deformation, and mandibular growth in juvenile idiopathic arthritis patients receiving systemic treatment. J Rheumatol. 2019 Sep 15. [Epub ahead of print] doi:10.3899/jrheum.190168
- Lochbühler N, Saurenmann RK, Müller L, Kellenberger CJ. Magnetic resonance imaging assessment of temporomandibular joint involvement and mandibular growth following corticosteroid injection in juvenile idiopathic arthritis. J Rheumatol. 2015 Aug;42(8):1514–1522.
- Stoll ML, Amin D, Powell KK, et al. Risk factors for intraarticular heterotopic bone formation in the temporomandibular joint in juvenile idiopathic arthritis. J Rheumatol. 2018 Aug;45(9):1301–1307.
- Stoustrup P, Kuseler A, Kristensen KD, et al. Orthopaedic splint treatment can reduce mandibular asymmetry caused by unilateral temporomandibular involvement in juvenile idiopathic arthritis. Eur J Orthod. 2013 Apr;35(2):191–198.
- Stoustrup P, Kristensen KD, Kuseler A, et al. Management of temporomandibular joint arthritis-related orofacial symptoms in juvenile idiopathic arthritis by the use of a stabilization splint. Scand J Rheumatol. 2014;43(2):137–145.
- Resnick CM, Frid P, Norholt SE, et al. An algorithm for management of dentofacial deformity resulting from juvenile idiopathic arthritis: Results of a multinational consensus conference. J Oral Maxillofac Surg. 2019 Jun;77(6):1152.e1–1152.e33.




