LONDON—Despite the detailed terminology for describing vasculitis established by the Chapel Hill Consensus (CHC) in 2012, the field badly needs better classification and diagnostic criteria for the group of diseases, an expert said in a presentation at the Annual Congress of the European League Against Rheumatism (EULAR 2016).
It’s a topic that is now being rigorously studied, with results likely coming in the next year or two, said Cees Kallenberg, MD, PhD, the former head of the department of rheumatology and immunology at the University Medical Center Groningen in The Netherlands, in a talk on the latest in the field.
The Vocabulary of Vasculitis
The umbrella term vasculitis—inflammation of the blood vessels that can affect a wide variety of organs—covers a broad range of diseases and syndromes based on vessel size, organ involvement and the likely causes. The groupings in the nomenclature from the CHC include large-, medium- and small-vessel vasculitis; single-organ vasculitis, such as cutaneous arteritis; primary central nervous system vasculitis; and those associated with probable etiologies, such as vasculitis associated with hepatitis B and drug-associated immune-complex vasculitis.
The problem with this vocabulary is that it “does not give diagnostic or even classification criteria,” Dr. Kallenberg said.
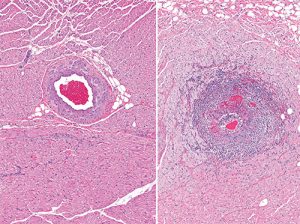
Severe inflammation of the artery (arteritis) (right) in the myocardium. For comparison, a normal healthy artery is shown on the left.
He gave an example from the 1990 American College of Rheumatology classification criteria to convey the need for improvements. The criteria for granulomatosis with polyangiitis (GPA) are nasal or oral inflammation; abnormal chest X-ray; microhematuria; and granulomatous inflammation on biopsy. If someone already has a diagnosis of vasculitis on histology and two of those four are present, a disease can be classified as GPA. But these criteria cannot be used as a diagnostic guide, Dr. Kallenberg said.
“If we use [these] criteria as diagnostic criteria, you must [diagnose] every patient with purulent nasal discharge and microhematuria [with] GPA, which is certainly not right,” he said. “So we definitely need better diagnostic and classification criteria.”
A large, multi-center, international prospective study—the DCVAS study—is underway to design and validate classification and diagnostic criteria, he noted.
ANCA+/-
Another big issue facing the field is whether ANCA-associated and ANCA-negative eosinophilic granulomatosis with polyangiitis (EGPA) should be considered as two different diseases, given that so many differences exist between the two. For example, the ANCA-associated form is typically a small-vessel vasculitis, while ANCA-negative is marked by tissue infiltration with eosinophils.
A Phase 3 study of the anti-IL5 antibody mepolizumab for EGPA is now underway, and the results might help further clarify the differences between the two subsets, Dr. Kallenberg said. Results are expected next year.
In another important development, recent studies looking at ANCA and other autoantibodies in infectious endocarditis and endocarditis-associated glomerulonephritis have found forms of ANCA were present more than a quarter of the time.1,2
“The lesson is, exclude infective endocarditis in every patient suspected of ANCA-associated vasculitis (AAV),” Dr. Kallenberg said.
In ANCA-associated vasculitis (AAV), the therapeutic aim of treatment without steroids could be coming closer to a reality. A Phase 2 study in AAV of the complement 5a receptor inhibitor, CCX168, compared those taking the drug with steroids to those taking the drug without steroids. Researchers found that a similar number in each group (86% vs. 81%) saw at least a 50% reduction in Birmingham Vasculitis Activity Score.3
A large, multi-center, international prospective study—the DCVAS study—is underway to design & validate classification & diagnostic criteria for vasculitis.
Systemic Sclerosis
John Varga, MD, director of the Northwestern Scleroderma Program, reviewed recent developments in precision treatment, genetics and treatments in systemic sclerosis.
A study published last year underscores the potential to select patients more effectively for certain treatments. The PANTHER trial in 2014 concluded that the amino acid N-acetylcysteine was no better than placebo in people with idiopathic pulmonary fibrosis. But a closer look at data from that trial, using genetics, found that those with a certain single nucleotide polymorphism (SNP) in the TOLLIP gene benefited, while in those with another it actually seemed to be harmful.4
Dr. Varga called this “one of the most intriguing and remarkable examples of precision medicine.”
Over the past year, research has shed new light on genetic variants that appear to have harmful effects related to systemic sclerosis. A new mutation identified in the phospholipid transporter gene ATP8B4, already identified as a risk for Alzheimer’s, also appears to be a damaging mutation in systemic sclerosis, but the function and the mechanism of action of this mutation aren’t known yet.5
A forthcoming study out of the University of California San Francisco using whole exome sequencing in diffuse cutaneous systemic sclerosis identifies several more mutations that appear damaging, but the effects of these are unknown as well.
So the challenge in this area, Dr. Varga said, will be to “establish the function and pathogenic role of genetic variants.”
Encouraging results have been collected recently for the use of rituximab, anti-IL6 tocilizumab and intravenous immunoglobulin (IVIg) in systemic sclerosis, offering the hope of more options to patients who fail first-line therapy, which Dr. Varga said remains mycophenolate mofetil.
In one of the more recent studies, refractory patients with active diffuse cutaneous systemic sclerosis were treated with IVIg, and the results were similar to those that MMF can produce, researchers found.6
But Dr. Varga emphasized that “Phase 3, randomized controlled trial data are needed.”
Thomas R. Collins is a freelance medical writer based in Florida.
References
- Mahr A, Batteux F, Duval X, et al. Brief report: Prevalence of antineutrophil cytoplasmic antibodies in infective endocarditis. Arthritis Rheumatol. 2014 Jun;66(6):1672–1677.
- Boils CL, Nasr SH, Walker PD, et al. Update on endocarditis-associated glomerulonephritis. Kidney Int. 2015 Jun;87(6):1241–1249. doi: 10.1038/ki.2014.424. Epub 2015 Jan 21.
- Jayne D. Successful steroid replacement in ANCA-associated vasculitis with C5a receptor inhibitor CCX168 in phase 2 randomized trial (CLEAR) Abstract No. MO039). 53rd European Renal Association—European Dialysis and Transplant Association (ERA-EDTA) Congress. Vienna, Austria. 2016 May 23.
- Oldham JM, Ma SF, Martinez FJ, et al. TOLLIP, MUC5B, and the Response to N-Acetylcysteine among Individuals with Idiopathic Pulmonary Fibrosis. Am J Respir Crit Care Med. 2015 Dec 15;192(12):1475–1482.
- Gao L, Emond MJ, Louie T, et al. Identification of rare variants in ATP8B4 as a risk factor for systemic sclerosis by whole-exome sequencing. Arthritis Rheumatol. 2016 Jan;68(1):191–200.
- Poelman CL, Hummers LK, Wigley FM, et al. Intravenous immunoglobulin may be an effective therapy for refractory, active diffuse cutaneous systemic sclerosis. J Rheumatol. 2015 Feb;42(2):236–242.