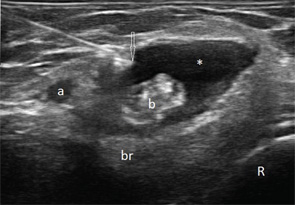
Figure 1
Transverse (see Figure 1) and longitudinal (see Figure 2) ultrasound images show an anechoic collection (asterisks),
which surrounds the distal biceps tendon (b). The collection is compressible (not shown here). The biceps tendon is heterogeneous in echo texture, with fiber dropouts and an irregular border (in the transverse view). The elbow joint does not show abnormalities (images not shown); hence, the collection was not felt to communicate with the joint. Aspiration of the collection was performed under ultrasound guidance (needle tip: arrow).
The ultrasound findings are consistent with bicipitoradial bursitis and distal bicep tendinosis. The distal biceps tendon is not covered by a synovial sheath, but rather by paratenon. Just proximal to its insertion to the radial tuberosity, the biceps tendon is in contact with the bicipitoradial (cubital) bursa, which does not communicate with the elbow joint but when distended can completely surround the biceps tendon and mimic tenosynovitis. Bicipitoradial bursitis should be distinguished from ganglion cysts, which may arise from the anterior elbow joint, connected via a pedicle, and expand distally.
Bicipitoradial bursitis can result from repetitive mechanical trauma, overuse, distal biceps tendon tear, tuberculosis,
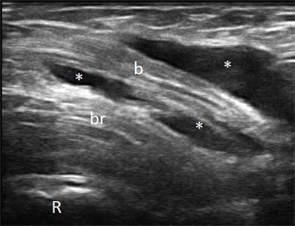
Figure 2
inflammatory arthritis, synovial chrondromatosis or amyloidosis. In our case the fluid was noninflammatory and crystal negative. Gram stain and culture, AFB smear and culture, cytology and Congo red stain were negative. The most likely reason for the bursitis remained overuse. Her symptoms improved with steroid injection and rest. Rarely, severe cases of bicipitoradial bursitis may require surgical resection of the bursa.
Ultrasound is useful in identifying bursitis, provides guidance for aspiration and injection, and allows for assessment of bicep tendon tear and macroscopic radial nerve damage resulting from compression.
Veronika Sharp, MD, is a faculty rheumatologist at the Santa Clara Valley Medical Center (SCVMC) in San Jose and is an affiliated clinical assistant professor at Stanford University, Palo Alto, Calif. She is director of musculoskeletal (MSK) ultrasonography in rheumatology at SCVMC.
Midori Jane Nishio, MD, is a rheumatologist in Walnut Creek, Calif., and is a volunteer faculty at SCVMC in MSK ultrasonography.
Lily Kao, MD, is a rheumatologist in San Jose, Calif., and is a volunteer faculty at SCVMC in MSK ultrasonography.
Send Us Your Images
Contact us at:
Simon Helfgott, MD
physician editor
E-mail: [email protected]
Keri Losavio
editor
E-mail: [email protected]