The most important serology test is the tTGA, and the higher the titer meaning the stronger the likelihood of celiac disease.
Controversy has arisen over the need for a biopsy in certain patients to make a diagnosis. The European Society of Pediatric Gastroenterology Hepatology and Nutrition has issued criteria saying that children could avoid a biopsy if they have symptoms suggesting the disease, if their tTGA is 10 times the upper normal limit and on a separate blood draw, if they are endomysial antibody positive and carry the HLA genes of either DQ2 or DQA. They also, of course, must respond to a gluten-free diet.
But others caution that some practitioners ignore these criteria. They also say that having a baseline histology can allow for the severity to be tracked, that some centers will not prescribe a gluten-free diet unless the diagnosis is proved and that a fully proved diagnosis has implications for family members, because up to 10% of first-degree relatives are affected.
Dr. Murray, along with Steffen Husby, MD, of Odense University Hospital in Denmark, has issued a kind of compromise approach: If the tTGA test is highly positive, then a positive endomysial test and positive HLA test means they can be considered to have celiac disease. If the tTGA test is negative, they probably do not have the disease. And if the tTGA is in the borderline range, then do a biopsy if their HLA test is positive. If the HLA test is negative, they can’t have the disease.
“So when you tell a patient your tTG is positive—your test for celiac is positive—say, ‘Please don’t start the gluten-free diet until you’ve got your biopsy done because it can go negative, especially in younger patients,’” Dr. Murray said.
Rheumatic diseases in which celiac disease is seen include inflammatory myositis, sarcoidosis, juvenile arthritis & primary Sjögren’s syndrome. Some patients also develop a fibromyalgia-like disorder, Dr. Murray said.
Dr. Murray said that a frequent misconception is that a positive HLA finding means that someone has the disease.
“Often that’s the most common problem I see: ‘Oh, my kids all have the genetic type; they’re all on a gluten-free diet.’ The parents have equated that with the disease, and that’s just not true,” he said.
Most people with the at-risk types will not have celiac disease, he said. Two-thirds of family members of those with the disease will carry the at-risk types, but most don’t get the disease.
Case Study
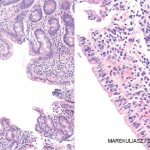
Sometimes, even a biopsy might not necessarily mean someone has celiac disease. In one of his cases, an 80-year-old woman came to him with a three-year history of occasional diarrhea and weight loss. She was gliadin antibody positive but tTG and endomysial antibody negative. A duodenal biopsy resulted in a celiac disease diagnosis.