
Valentyn Volkov / shutterstock.com
Idiopathic inflammatory myopathies are heterogenous, acquired immune-mediated muscle diseases. Over the past decade, immune-mediated necrotizing myopathy has been recognized as a subcategory of idiopathic inflammatory myopathy characterized by myofiber necrosis in the absence of prominent inflammatory cells.1 Autoantibodies against signal recognition particle (SRP) and 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR) are thought to be associated with the development of immune-mediated necrotizing myopathy. The latter was originally identified in patients exposed to statin in the U.S. and was initially thought to be specific to statin-associated necrotizing myopathy.2 In East Asia, however, the rate of statin-naive immune-mediated necrotizing myopathy seems to be much higher than in North America.3-5
In this article, we present a case of statin-naive, anti-HMGCR and anti-SRP antibody-positive immune-mediated necrotizing myopathy possibly associated with the daily ingestion of shiitake mushrooms (Lentinula edodes).
Case Report
A 73-year-old man visited our hospital because of myalgia and a high serum creatine kinase (CK) level (1,169 IU/L). Eight months previously, his CK was found to be high at a routine health checkup. Five months previously, he had developed diffuse myalgia over the shoulders, back and thighs. He also noted mild difficulty climbing up stairs, but otherwise he did not notice any muscle weakness. He denied fever, weight loss, joint pain, skin rash, Raynaud’s phenomenon, cough or dyspnea. He had a past medical history of hypertension, gastric ulcer, and lumbar disc herniation. He was taking amlodipine, but had never taken a statin.
Our patient worked as a forester. He drank a moderate amount of Japanese sake and had quit smoking 10 years prior. Of note, he had been growing shiitake mushrooms in his garden for five years, and he ate them almost every day, especially in spring and autumn, the harvest season. He ate two to three mushrooms a day on average.
A physical examination showed his vital signs were within normal limits. Auscultation of lungs and heart was normal. He had muscle tenderness over his back and both thighs. Manual muscle testing revealed mild weakness only in the hip flexors (4/5 on the medical research council scale), but he had normal strength in the rest of his muscles.
On laboratory tests (see Table 1), his serum CK level was 1,280 IU/L. Anti-nuclear antibody immunofluorescence staining showed cytoplasmic pattern (1:80). Anti-Jo-1 and other selected autoantibodies were negative.
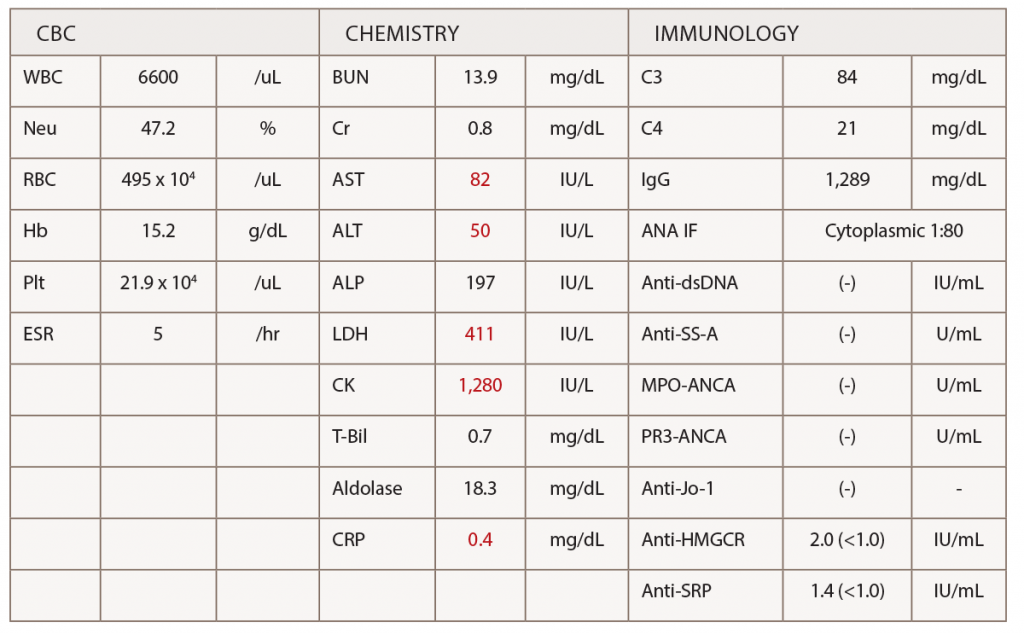
(click for larger image) Table 1: Laboratory Tests
Abbreviations: ANA IF; antinuclear antibody immunofluorescence staining, Anti-dsDNA; anti-double strand DNA antibody, MPO-ANCA; myeloperoxidase anti-neutrophil cytoplasmic antibody, PR3-ANCA; proteinase-3 anti-neutrophil cytoplasmic antibody.
A magnetic resonance imaging scan of his arms and legs did not reveal any abnormalities. A needle electromyography did not show signs of irritable myopathy.
Despite these unremarkable test results, we suspected immune-mediated necrotizing myopathy based on otherwise unexplainable myalgia and CK elevation, as well as the history of daily consumption of shiitake mushrooms. We performed muscle biopsy of the left biceps brachii and obtained blood for further analysis for autoantibodies associated with idiopathic inflammatory myopathies.
The muscle biopsy (see Figure 1) showed one necrotic and several internally nucleated fibers, in addition to moderate upregulation of MHC class I staining, raising a possibility of immune-mediated necrotizing myopathy—albeit complement C5b-9 was not deposited on the sarcolemma. The autoantibody analyses using enzyme-linked immunosorbent assay (ELISA) revealed both anti-HMGCR and anti-SRP antibodies were positive (antibody titer 2.0 IU/mL and 1.4 IU/mL, respectively; cutoff 1.0 IU/mL).
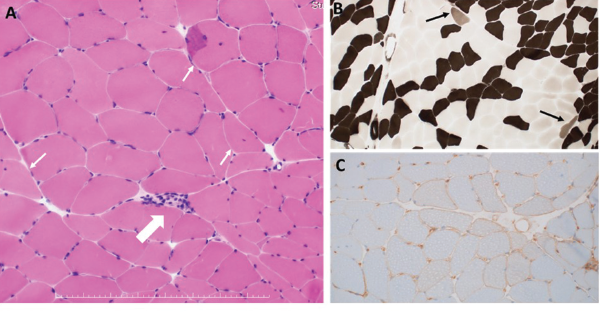
Figure 1: Histopathological Findings of Left Biceps Brachii
A: HE staining. One necrotic fiber was observed (large arrow). Some muscle fibers with internal nuclei were observed (small arrow). B: ATPase staining. A few type 2C fibers were observed (arrows). C: MHC Class I staining. Moderate upregulation of sarcolemmal MHC class I molecule was seen.
A diagnosis of immune-mediated necrotizing myopathy associated with these two antibodies was made. We started 50 mg a day of prednisolone orally, as well as cessation of mushroom intake. His symptoms and CK levels quickly improved. We tapered the prednisolone and started azathioprine. Although we discontinued azathioprine because of side effects, his symptoms remained stable. Eighteen months later, we successfully discontinued prednisolone and are now observing his symptoms without treatment.
In East Asia, the rate of statin-naive, anti-HMGCR antibody-positive immune-mediated necrotizing myopathy is much higher than in North America, raising a possibility that different triggering materials may be associated with immune-mediated necrotizing myopathy.
Discussion
Statins are believed to trigger autoantibody production against HMGCR in individuals who have a susceptibility.8 Regenerating fibers are known to overexpress HMGCR. Therefore, statin-induced myofiber necrosis and generation may well provide more antigens to produce pathogenic autoantibodies, creating a feed-forward loop.2,7 The binding of statins to HMGCR may also change the conformation of the protein, leading to the generation of new epitopes to which the immune system is not tolerant.2
In East Asia, the rate of statin-naive, anti-HMGCR antibody-positive immune-mediated necrotizing myopathy is much higher than in North America, raising a possibility that different triggering materials may be associated with immune-mediated necrotizing myopathy—especially in patients in East Asia.3-5 In this regard, it may be an attractive hypothesis that the foods containing natural HMGCR inhibitors, such as shiitake mushrooms, red yeast rice and pu’erh tea (a variety of fermented tea), which are apparently consumed more frequently in the region, trigger the disease in this statin-naive population. Further, infantile-onset immune-mediated necrotizing myopathy associated with anti-HMGCR autoantibodies has been found in patients from Japan.6 This is interesting considering shiitake mushrooms are often used as a weaning food in Japan.
Although shiitake mushrooms have been shown to have an inhibitory effect on HMGCR, the specific molecule responsible for this effect has not been found. Gil-Ramirez, et al. showed that among water extracts obtained from 26 different mushroom species, Lentinula edodes was one of the strongest in exerting HMGCR inhibitory activity.9 The same authors also reported that the administration of extracts from Lentinula edodes to mice modulated the transcriptional profile of genes involved in the cholesterol metabolism, similarly to simvastatin, indicating shiitake mushrooms exert inhibitory activity on HMGCR similar to that of statins and may well trigger autoimmunity to HMGCR just as statins do.10
In the case presented here, simultaneous cessation of mushroom ingestion and treatment with glucocorticoids and an immunosuppressive agent led to complete remission of disease activity. Successful treatment of anti-HMGCR antibody-positive immune-mediated necrotizing myopathy usually requires not only cessation of the offending agent but also treatment with immunosuppressive agents, just as in this case.2,10
Our patient showed the presence of both of anti-HMGCR and anti-SRP antibodies. Although these two autoantibodies are considered to be mutually exclusive, the ELISA system we used has very high specificity in detecting both of them.11 In a large case series in Japan, among 387 patients with idiopathic inflammatory myopathies other than inclusion body myositis, the frequencies of anti-SRP and anti-HMGCR antibodies were 18% and 12%, respectively, and only one patient had both autoantibodies. Details of this case were not discussed in the literature.4 We need to wait for more reports of similar cases to know the exact pathomechanism of co-existence of these two antibodies.
Conclusion
In summary, we presented a case of an elderly man with statin-naive immune-mediated necrotizing myopathy positive for both anti-HMGCR and anti-SRP autoantibodies. Anti-HMGCR antibody-positive immune-mediated necrotizing myopathy may be associated with exposure to naturally occurring dietary HMGCR inhibitors as well as statins. For successful treatment of anti-HMGCR immune-mediated necrotizing myopathy, both cessation of the offending agent and treatment with glucocorticoids and immunosuppression are often necessary.
Physicians need to consider not only the patient’s medical and social history, but also their dietary history when evaluating patients suspected to have immune-mediated necrotizing myopathy.
Takeshi Yoshida, MD, Hiroaki Chikazawa, MD, and Yoshitaka Kumon, MD, PhD, all work in the Department of Rheumatology at Chikamori Hospital, Kochi, Japan.
Ichizo Nishino, MD, PhD, is the director of the Department of Neuromuscular Research at the National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan.
Call for Cases
The 2019 Thieves Market Call for Cases is now open. Find more information on the ACR website.
Disclosure
This study was supported in part by Intramural Research Grant (29-4) for Neurological and Psychiatric Disorders from the National Center of Neurology and Psychiatry.
References
- Stenzel W, Goebel HH, Aronica E. Review: Immune-mediated necrotizing myopathies—a heterogeneous group of diseases with specific myopathological features. Neuropathol Appl Neurobiol. 2012 Dec;38(7):632–646.
- Mammen AL. Statin-associated autoimmune myopathy. New Engl J Med. 2016 Feb 18;374(7):664–669.
- Mammen AL, Chung T, Christopher-Stine L, et al. Autoantibodies against 3-hydroxy-3-methylglutaryl-coenzyme A reductase in patients with statin-associated autoimmune myopathy. Arthritis Rheum. 2011 Mar;63(3):713–721.
- Watanabe Y, Uruha A, Suzuki S, et al. Clinical features and prognosis in anti-SRP and anti-HMGCR necrotising myopathy. J Neurol Neurosurg Psychiatry. 2016 Oct;87(10):1038–1044.
- Klein M, Mann H, Pleštilová L, et al. Increasing incidence of immune-mediated necrotizing myopathy: Single-centre experience. Rheumatology (Oxford). 2015 Nov;54(11):2010–2014.
- Liang WC, Uruha A, Suzuki S, et al. Pediatric necrotizing myopathy associated with anti-3-hydroxy-3-methylglutaryl-coenzyme A reductase antibodies. Rheumatology (Oxford). 2017 Feb;56(2):287–293.
- Selva-O’Callaghan A, Alvarado-Cardenas M, Pinal-Fernández I, et al. Statin-induced myalgia and myositis: An update on pathogenesis and clinical recommendations. Expert Rev Clin Immunol. 2018 Mar;14(3): 215–224.
- Ohnuki Y, Suzuki S, Shiina T, et al. HLA-DRB1 alleles in immune-mediated necrotizing myopathy. Neurology. 2016 Nov 1;87(18):1954–1955.
- Gil-Ramírez A, Clavijo C, Palanisamy M, et al. Screening of edible mushrooms and extraction by pressurized water (PWE) of 3-hydroxy-3-methyl-glutaryl CoA reductase inhibitors. J Funct Foods. 2013 Jan;5(1):244–250.
- Gil-Ramírez A, Caz V, Smiderle FR, et al. Water-soluble compounds from Lentinula edodes influencing the HMG-CoA reductase activity and the expression of genes involved in the cholesterol metabolism. J Agric Food Chem. 2016 Mar 9;64(9):1910–1920.
- Ikemoto K, Suzuki S, Uruha A, et al. Enzyme-linked immunosorbent assays for diagnosis of immune-mediated necrotizing myopathy. Clin Exp Neuroimmunol. 2016 Aug;7(3):291–293.


