CHICAGO—The 2018 ACR/ARHP Annual Meeting session on genetic mimics of rheumatic disease began with a description of a patient who presented with the symptoms of childhood-onset lupus but instead had a well-defined genetic disease: lysinuric protein intolerance (LPI).
CHICAGO—The 2018 ACR/ARHP Annual Meeting session on genetic mimics of rheumatic disease began with a description of a patient who presented with the symptoms of childhood-onset lupus but instead had a well-defined genetic disease: lysinuric protein intolerance (LPI).
Lindsay Burrage, MD, PhD, assistant professor of molecular and human genetics at Baylor College of Medicine, Houston, used that anecdote in her presentation as an example of the overlap between inborn errors of metabolism and rheumatology. She explained that the immune system and metabolism are highly integrated. As a result, the clinical signs and symptoms of metabolic derangement can overlap with rheumatic disease. She discussed the presentation and appropriate diagnostic testing for LPI and reviewed the metabolic differential diagnosis.
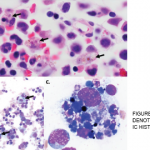
LPI can present with a variety of features, including failure to thrive, osteoporosis, pulmonary alveolar proteinosis, renal disease, immunodeficiency, autoimmunity, macrophage activation syndrome or hemophagocytic lymphohistiocytosis, and secondary urea cycle dysfunction. It is caused by pathogenic variants in SLC7A7, which encodes an amino acid transporter. Although Dr. Burrage acknowledged it is not possible to check all patients who present with symptoms of lupus for metabolic disorders, clues suggestive of LPI include short stature, failure to thrive, macrophage activation and protein alveolar proteinosis. Mild developmental delay and significant fractures may also be red flags. Providers can screen for LPI using plasma and urine amino acids and a plasma ammonia level.
Dr. Burrage also discussed Fabry disease, which is caused by pathogenic variants in the gene GLA encoding α-galactosidase A. Fabry disease has an incidence of 1:40,000–1:117,000, and patients can experience pain crises associated with fever and elevated erythrocyte sedimentation rate (ESR). In fact, the initial presenting feature of Fabry disease is often an acute and chronic pain crisis that involves the extremities, and patients may be referred to rheumatologists for evaluation of the cause for this pain. Unfortunately, the disorder is notorious for delayed diagnosis, which can impact treatment.
Other genetic metabolic disorders can also mimic rheumatologic diseases, and Dr. Burrage emphasized the importance of recognizing these diagnoses because successful diagnosis facilitates early initiation of targeted therapies, genetic counseling for families and testing of at-risk family members.
Genetic diagnoses should be considered in the differential diagnosis of early onset arthritis.
Mahim Jain, MD, assistant professor of pediatrics at Johns Hopkins School of Medicine, Baltimore, took the stage to discuss connective tissue and bone disorders. He explained that because genetic connective tissue disorders affect collagen, they can present as arthritis, and he used Ehlers-Danlos syndromes (EDS) as an example. EDS is a collection of hypermobility syndromes that can prove difficult to diagnose, especially because approximately 10% of the adult population has hypermobility.
Dr. Jain stated that because arthritis can be a feature of certain genetic conditions, genetic diagnoses should be considered in the differential diagnosis of early onset arthritis. He noted that he conducts panel tests for EDS genes on such patients and performs even more detailed testing on patients with a complicated clinical history. Dr. Jain follows patients with EDS, seeing them every three to six months. He recommends they undergo regular ophthalmology evaluations and encourages joint sparing activities such as swimming and aquatic physical therapy. He also noted that patients with EDS will likely need strategies to help address their pain.
The final speaker of the session, Brian A. Cobb, PhD, professor of pathology at Case Western University, Cleveland, Ohio, described congenital disorders of glycosylation. The focus of his talk was the connection between glycans, the immune response and rheumatic disease.
Dr. Cobb began with an overview of glycosylation, describing it as the most common biological modification to proteins. He explained that proteins can be glycosylated in several ways, O-glycosylation and N-glycosylation being the most abundant. O-glycosylation happens post-translationally as a host of enzymes decorate proteins with a complex array of glycans. In the case of N-glycosylation, however, carbohydrates are covalently attached to free nitrogen on arginine via the transfer of a precursor glycan. The terminal glycans are then cleaved off in the endoplasmic reticulum. Once the glycans are removed, the protein is shuttled into the Golgi apparatus where it gets further broken down and rebuilt into complex structures.
N-glycosylation is important for protein folding control, and Dr. Cobb emphasized that these glycosylation enzymes determine the regulation and the nature of the carbohydrate structures, including receptors for chemokines, that are presented on the cell surface or secreted by cells. The process requires an entire metabolic pathway coded for by approximately 2% of the genome and is very much linked to the metabolic state of the cell.
Patients with congenital disorders of glycosylation (CDG), such as ALG12-CDG, experience recurring infections, and decreased serum immunoglobulin (Ig)G, IgA and IgM. They also have decreased numbers of B cells and fail to make antibody responses to diphtheria and other vaccine antigens. In contrast, patients with MAGT1-CDG have mild primary combined immune deficiency, persistent elevation of viral load in Epstein-Barr virus and increased incidence of B cell lymphomas.
Dr. Cobb explained that rheumatologists should not only be aware that patients may have CDG’s, but also realize the glycosylation pathways could influence the efficacy of antibody-based biologics because glycosylation enzymes circulate in the bloodstream and change in concentration as a function of inflammation. Because such glycosylation can affect therapeutic antibody function, therapeutic antibodies should be engineered and tested to limit the extent of potential modifications and maximize efficacy.
Lara C. Pullen, PhD, is a medical writer based in the Chicago area.