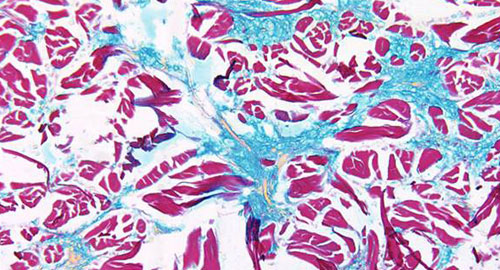
 Patients with scleroderma can have a wide range of autoantigens, and distinct autoantigen profiles seem to correlate with a specific course of disease. Scleroderma is most frequently associated with the autoantibodies, anti-centromere, anti-topoisomerase 1 and anti-RNA polymerase III (anti-POLR3). Patients with all three of these autoantibodies can be described as anti-CTP antibody positive. Some patients with scleroderma are also anti-CTP antibody negative. Often, these individuals rapidly go on to develop cancer. The details of their autoimmune response and its relationship to cancer remain unknown.
Patients with scleroderma can have a wide range of autoantigens, and distinct autoantigen profiles seem to correlate with a specific course of disease. Scleroderma is most frequently associated with the autoantibodies, anti-centromere, anti-topoisomerase 1 and anti-RNA polymerase III (anti-POLR3). Patients with all three of these autoantibodies can be described as anti-CTP antibody positive. Some patients with scleroderma are also anti-CTP antibody negative. Often, these individuals rapidly go on to develop cancer. The details of their autoimmune response and its relationship to cancer remain unknown.
George J. Xu, PhD, a graduate student at Harvard University in Cambridge, Mass., and colleagues addressed this knowledge gap with their analysis of intramolecular epitope spreading in patients with scleroderma. Their precision medicine approach allowed them to meet the challenges presented by a complex autoimmune response. They published the results online last November in the Proceedings of the National Academy of Sciences.1
“To address these issues, we have developed and used two high throughput epitope identification methods to identify immunological characteristics of different subclasses of scleroderma (POLR3-positive scleroderma with cancer, POLR3-positive scleroderma without cancer and patients with cancer-associated scleroderma who are anti-CTP–negative),” write the authors in their discussion. “Our methods included a significantly improved version of PLATO [parallel analysis of translated ORFs], PLATO-BC, which greatly simplifies the original assay, which was not compatible with high-throughput applications.” The investigators combined a bar-coded whole-genome ORF mRNA display library with phage-immunoprecipitation sequencing (PhIP-Seq). They used the approach to analyze sera from patients with scleroderma with or without known autoantibody specificities.
The researchers were able to successfully identify the POLR3 complex in cancer-associated scleroderma using PhIP-Seq. They also found notable intermolecular spreading among subunits of the POLR3 complex. Approximately one-quarter of patients with scleroderma and cancer did not have antibodies to CTP, but did have autoantibodies against the minor spliceosome complex. These patients had autoantibodies to RNA Binding Region (RNP1, RNA recognition motif) Containing 3 (RNPC3), as well as various other components of the minor spliceosome. This specificity was absent in unrelated autoimmune diseases. The investigators also found intra- and intermolecular epitope spreading within RNPC3 and the complex.
“Our results demonstrate the benefit of combining the two complementary approaches, PhIP-Seq and PLATO-BC, for identifying autoantibody specificities in large, heterogeneous populations,” explained the authors. “These methods have complementary strengths and weaknesses. Although PhIP-Seq has the advantages of being high throughput, identifying individual epitopes, detecting intraprotein epitope spreading and possessing a complete representation of the human proteome, it does not identify all patients with a particular specificity (e.g., POLR3A), possibly due to its reduced ability to detect a portion of antibodies that recognize discontinuous epitopes.”
They concluded that, when combined, the two technologies are useful for stratifying patients and discovering pathogenic pathways.
Lara C. Pullen, PhD, is a medical writer based in the Chicago area.
Reference
- Xu GJ, Shah AA, Li MZ, et al. Systematic autoantigen analysis identifies a distinct subtype of scleroderma with coincident cancer. Proc Natl Acad Sci USA. 2016 Nov 22;113(47):E7526–E7534. Epub 2016 Nov 7.