It is well known that hip fractures are associated with significant morbidity and mortality: Mortality increases 15–25% in the year following a hip fracture.1–5 We know that treating osteoporosis prevents fractures and improves patient survival. But is there a relationship beyond this?
Several studies have found that bisphosphonate therapy is associated with a reduction in both all-cause and cardiovascular (CV) related mortality beyond what would be expected by preventing the next fracture. However, the data are not conclusive. What do the data say, and how should we advise our patients?
Bisphosphonate Use & Mortality
Prospective cohort studies, meta-analyses and randomized, controlled trials have demonstrated that bisphosphonate use is associated with a reduction in all-cause mortality.1,6,7–15 Although the majority of studies are observational, data from a variety of studies in different clinical settings demonstrate reduced all-cause mortality among patients taking bisphosphonate therapy. Before discussing the more focused question of CV-related morbidity and mortality, we briefly review the most compelling data demonstrating a connection between bisphosphonate use and all-cause mortality.
A large systematic review and meta-analysis conducted by Cummings et al. in 2019 investigated a bold question: If bisphosphonates are associated with decreased mortality, then should they be administered to patients for the mortality benefit alone?16 This study examined 21 clinical trials of bisphosphonate use and did not find an overall association between bisphosphonate use and all-cause mortality.16 However, a trend toward lower mortality associated with nitrogen-containing bisphosphonate use was seen in 20 trials.
Six trials of zoledronic acid showed marked heterogeneity. Some studies, such as the Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly-Recurrent Fracture Trial (HORIZON-RFT), observed a substantial reduction in the risk of death, but others did not.1 Ultimately, Cummings et al. concluded that bisphosphonate use may not be associated with reduced overall mortality rates, but additional trials are needed to clarify mortality rates associated with zoledronic acid use.
One of several limitations to this study was the exclusion of patients on glucocorticoids and patients with cancer. Even though a discussion of all clinical trials addressed in the Cummings study is beyond the scope of this article, we address some of the more compelling trials below.
View 1
Bisphosphonate Use Is Associated with a Reduction in All-Cause Mortality
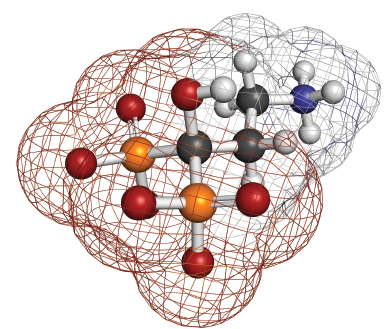
A representation of pamidronic acid, a bisphosphonate used to treat osteoporosis.
The HORIZON-RFT trial demonstrated that zoledronic acid use was associated with an absolute fracture reduction of 5.3% and a relative reduction of 35% compared with the placebo group (primary endpoint). Beyond this, zoledronic acid use was associated with a 28% relative reduction in the risk of death among patients with recent surgical repair of a hip fracture, a mortality benefit that persisted after controlling for baseline factors between individuals who received zoledronic acid and those who did not (secondary endpoint).1
Interestingly, as we discuss below, only 8% of the 28% reduction in risk of death was related to a reduction in hip fracture, implying that prevention of secondary fracture does not entirely explain the reduction in mortality risk.12 The mortality benefit seen with zoledronic acid use in HORIZON-RFT was unexpected and launched efforts to confirm and explain this finding. Of note, the number of CV events was similar between the two groups.1
Additional studies have likewise shown an improvement in all-cause mortality among bisphosphonate users. A smaller Canadian trial, drawing on patients previously randomized to either care manager intervention (i.e., arrangement for bone mineral density testing and oral bisphosphonate prescription) or usual care, demonstrated a significant reduction in mortality among patients on bisphosphonates.8
Using data from the West Glasgow health service between 1999 and 2007, a prospective cohort study demonstrated a decreased risk of mortality among patients receiving oral bisphosphonates compared with those taking just calcium and vitamin D.15 Interestingly, this study was conducted among patients who were referred to a fracture liaison service following a fragility fracture, arguably a more generalizable and real-world population than that represented by a randomized, controlled trial.15
A meta-analysis of eight studies published in 2010 found that treatment with osteoporosis therapy among 40,000 subjects—including oral and intravenous bisphosphonates—resulted in a 10% reduction in mortality.9 This observation was most prominent among patients at highest risk of fracture.9