I went to medical school for the reason that most people go to medical school—to help people. And I chose rheumatology probably for the same reason that a lot of rheumatologists chose rheumatology— because I had a mentor who stimulated my interest in rheumatology. The experience of working with our courageous patients with chronic musculoskeletal disorders has been as fulfilling as I had hoped it would be when I started out 30 years ago.
So why is it that some days I feel more like an accountant than a rheumatologist?
Coding and documentation rules continue to be a bouncing ball of changes, and physicians have to continually follow minute rules that make you feel like you’re analyzing the internal revenue code. And while some changes may have offered some benefits to practice in the past, recent changes haven’t—and what’s coming down the pike in 2010 just might be the worst we’ve yet to experience.
Consult Coding in 2010
What’s new for 2010? If you have had problems distinguishing between new patients and consultations, have no fear. Consultation codes have been eliminated effective January 1, 2010. Physicians will only be able to report for new and established visits. The Centers for Medicare and Medicaid Services (CMS) decided to eliminate consultation codes because there appeared to be a correlation between the complexity of the codes and the level of errors made by submitting physicians. True, life would be much easier without thousands of current procedural terminology and diagnosis codes. Unfortunately, eliminating consultation codes reduces payment for specialists who must take extra time reviewing thick charts and diagnosing patients with complex medical situations. CMS is taking the money that would have been spent on consults and reallocating the money into new and established evaluation and management codes, increasing the reimbursement for these codes. This will provide a small increase of reimbursement for all physicians who perform evaluation and management procedures without recognizing the additional work performed by specialists.
And although CMS has eliminated consults, insurance companies have not determined what they are going to do. The Current Procedural Terminology (CPT) editorial panel has not deleted the codes from the CPT book, so the codes still exist. The question is, will non-Medicare carriers continue to recognize consultation codes? What happens when patients have secondary insurance? The coding and billing staff will have to be vigilant to determine if the consult code is valid at a particular insurance company. The administrative burden of coding continues.
To date, the ACR has been fighting the elimination of consultation codes at multiple levels without success. At the recent American Medical Association (AMA) meeting, Gary Bryant, MD, and Eileen Moynihan, MD—the ACR’s AMA delegate and alternate delegate, respectively—submitted a resolution at the House of Delegates for the AMA to support legislation to reverse the elimination of consultation codes. Many specialties supported the resolution, which became AMA policy at the end of the meeting. The ACR, along with the AMA and other specialties, will now continue to pursue legislation so that consultation will not be eliminated. It is hoped that language to restore consultation codes will be added to a bill to reform Medicare’s Sustainable Growth Rate as the bill moves forward and hopefully passes.
Challenges on Other Fronts
Individual insurance company rules continue to plague physicians. For example, Trailblazer—the Medicare carrier for Texas and a few other states— recently released a memorandum to assist physicians in understanding the level of complexity for these codes, stating that this is the “bottom line” for evaluation and management codes. Trailblazer advises physicians not to code using the highest two codes when “fewer than three distinct medical conditions/complaints were evaluated and managed during the encounter.” This is substantively different from the level of complexity specified by CMS nearly 20 years ago, and physicians have all gone to great lengths to understand and abide by what constitutes different levels of complexity needed to justify our billing. I like things simplified as much as the next person, but what is the thought process behind such a dramatic change in the understanding of the work necessary to justify a level of billing? A typical rheumatoid arthritis or lupus patient generally has enough complexity to justify higher coding without requiring that three distinct medical conditions be evaluated and managed. To me, it seems as though Trailblazer is arbitrarily raising the bar to make it more difficult for practitioners to fulfill the complexity required for higher billing codes. The ACR has sent a letter to Trailblazer urging it to follow CPT rules.
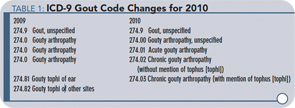
Physicians must also monitor changes to International Classification of Diseases (ICD) codes as well. On October 1, 2009, several rheumatologists were surprised to find out that gout codes had been modified from one code to four codes. If you reported the previous gout ICD-9 code, your bill will be denied. The books that provide the updates for over 13,000 codes were sent to the ACR in early October. I am sure that most physician offices received their books at the same time, not giving anyone adequate time to review the information and determine what changes would affect their practice. It is also confusing that ICD-9 changes go into effect on October 1 each year and CPT changes are effective January 1. This allows the physician practice to be disrupted on a more frequent basis. Superbills must be modified twice a year instead of just once for the year. Gout codes will see more changes next year. See Table 1 (below) for the ICD-9 gout code changes for 2010.
New Coding Manual on the Horizon
ICD-10 is around the corner. The United States is slated to move to ICD-10 in 2013. Many other countries have been using ICD-10 for several years and are currently preparing for ICD-11. The United States is behind because of the cost and training issues related to moving to ICD-10. Some reports have listed the cost for a single practice to upgrade to ICD-10 to be as high as $85,000. This is quite a steep price tag to report a diagnosis based on a number. The change from ICD-9 to ICD-10 is going to substantially increase the number of diagnosis codes.
There are proponents and opponents on both sides of the argument to move to ICD-10. I care about how it is going to affect my practice. In my practice, we are currently halfway through the process of moving our entire group to an electronic medical record. Presumably all the software will have to be updated at a cost to our practice. The coding and billing staff will have to be retrained, as will physicians who long ago memorized the 20 or 30 codes that we most commonly bill. It will lead to a disruption in the practice, which will also decrease reimbursement. This is yet another administrative burden to shoulder.
Why did I become a physician? Certainly not to constantly reinterpret complex coding and documentation rules. Do the patients care what code relates to their diagnosis or procedure? No. This is just another example of excessive administrative work that takes away from the focus of physicians to provide care for their patients. Although the ACR supports reform of the healthcare system, we remain increasingly concerned with the continued increase in the administrative burden in an environment of decreasing reimbursement. The ACR, along with other specialty societies, will continue to fight for our physicians to improve the delivery process and maintain adequate reimbursement so that they can provide the services necessary to ensure quality care. When the dust settles, hopefully the best interests of our patients will be the driving force for change, not the budget.
Dr. Cohen is president of the ACR. Contact him via email at [email protected].