Updates from the ACR Convergence 2023 Review Course, part 4

The Review Course drew quite the crowd on Saturday morning at ACR Convergence 2023.
SAN DIEGO—Under the leadership of moderators Noelle Rolle, MBBS, assistant professor in the Division of Rheumatology, associate program director of the Rheumatology Fellowship at the Medical College of Georgia, Augusta University, and Julia Schwartzmann-Morris, MD, associate professor, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Great Neck, N.Y., the one-day Review Course held before ACR Convergence 2023 officially kicked off on on Saturday, Nov. 11, covered a plethora of important topics.
Relapsing Polychondritis
Marcela Ferrada, MD, who most recently was on faculty with the National Institutes of Health (NIH), Bethesda, Md., discussed relapsing polychondritis (RP), a condition that she herself has and for which she serves as a passionate advocate.
RP is a rare, heterogeneous, systemic inflammatory disease that targets cartilage. The diagnosis is a clinical one and commonly involves auricular chondritis, and redness and pain of the cartilaginous structures of the nose. Dr. Ferrada made a point of noting that the nose in these patients can look normal, but can still be quite painful; she also explained that we still are without a formal system of defining and grading ear chondritis.
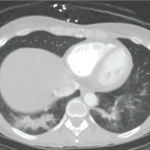
Patients with RP may have upper airway disease, in the form of subglottic stenosis, or lower airway disease, which can manifest with tracheomalacia. Bronchial obstruction can also occur in some patients. With regard to musculoskeletal manifestations, a non-erosive arthritis can occur, although Dr. Ferrada suspects this may actually be a form of tenosynovitis rather than a true arthritis. Patients with RP may, uncommonly, experience severe scleritis; episcleritis is more common and typically less severe. There can also be inner ear involvement, with subsequent hearing loss and tinnitus.
Diagnosis
Dr. Ferrada shared a number of clinical pearls that help clarify misunderstandings about diagnosing RP. First, she noted that antibodies against type II collagen are not of much utility; in fact, the initial report of the possible association of these antibodies with RP was from an article in the 1970s that included only 15 total patients.
Second, biopsy is not required to diagnose RP, but it can be helpful and sometimes necessary to exclude infections or other diseases if they are suspected. This is an important point because performing a biopsy in a patient with RP can trigger a flare of the disease.