Third, inflammatory markers can be normal in patients with RP, even when the disease is active, thus a normal erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) does not rule out the diagnosis.
Typing RP
Dr. Ferrada presented compelling data to show that what we call RP may actually be more than one disease, or at the very least has several distinct subtypes. In a landmark paper on the subject, Dr. Ferrada and colleagues identified three subtypes of RP.
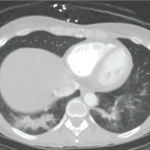
Type 1 RP is less common, but can be severe and is characterized by chondritis, tracheomalacia, saddle-nose deformity and subglottic stenosis. These patients tended to have the shortest time to diagnosis, highest disease activity and most frequent need for intensive care unit admission and tracheostomy.
Type 2 RP is characterized by tracheomalacia and bronchomalacia, but not saddle-nose deformity or subglottic stenosis; these patients have the longest time to diagnosis.
Type 3 RP is characterized by tenosynovitis/synovitis and ear chondritis.1
Across all three subtypes of patients, it is important to ask about a history of oral and genital ulcers; some of these patients may actually have a condition called mouth and genital ulcers with inflamed cartilage (MAGIC) syndrome. On that note, the presence of oral and genital ulcers may also imply the possibility of Behçet’s disease, although this condition does not normally have cartilaginous involvement as well.
Dr. Ferrada made note of the work from Dion and colleagues in 2016 that identified a subgroup of patients with RP with unusual hematologic findings.2 These data were shown to be significant in 2020 with the first description of VEXAS syndrome, which is an adult-onset inflammatory syndrome due to a somatic mutation in the UBA1 gene that can present with fevers, cytopenias, vacuoles in myeloid and erythroid precursor cells, dysplastic bone marrow, neutrophilic cutaneous and pulmonary inflammation, chondritis and vasculitis.3 It is estimated that about 8% of patients with RP have VEXAS and about 60% of patients with VEXAS have RP. Thus, if you see a patient with ear and nose chondritis with a mean corpuscular volume (MCV) greater than 100 fL and a platelet count less than 200,000/μL of blood, it’s important to highly consider the possibility of VEXAS and refer for genetic testing.
Treatment
In terms of treatment for RP, Dr. Ferrada noted that, unfortunately, a standard of care does not exist at present. Medications that are frequently used include corticosteroids, methotrexate, mycophenolate mofetil, leflunomide, TNF-α inhibitors and interleukin-6 (IL-6) inhibitors. Dapsone has been used in patients, but Dr. Ferrada prefers to avoid this medication because it can cause hemolytic anemia and methemoglobinuria.