Tupungato; Svetlana Voronova/shutterstock.com
The levels of service within an evaluation and management (E/M) visit are based on the documentation of key components, which include history, physical examination and medical decision making. The history component is comparable to telling a story and should include a beginning and some form of development to adequately describe the patient’s presenting problem.
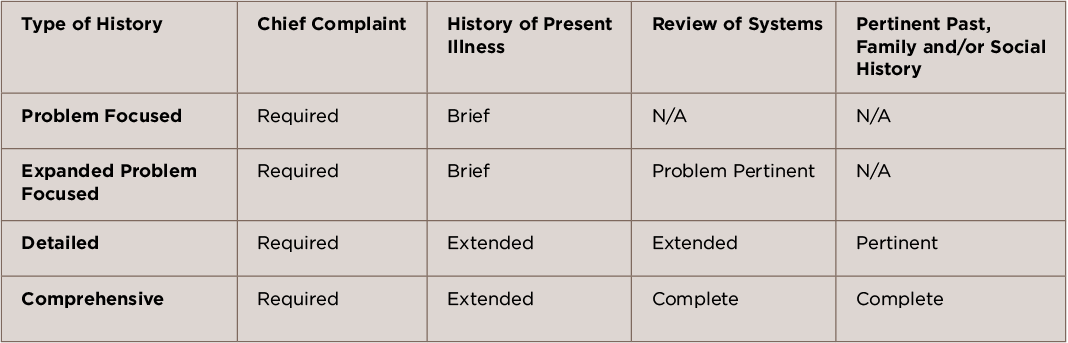
To ensure high-quality patient care and proper reimbursement, it is important that documentation of the history element tell the complete story of why the patient is in the office. The Centers for Medicare and Medicaid Services (CMS) Documentation Guidelines for Evaluation and Management Services have four history levels, each of which comprises four elements.1 To qualify for a given history level, certain elements are required, as depicted in Table 1.
Note from the table that as the type of history becomes more intensive, the elements required to perform that type of history also increase in intensity. For example, a problem-focused history requires documentation of the chief complaint (CC) and a brief history of present illness (HPI), while a detailed history requires the documentation of a CC, an extended HPI, plus an extended review of systems (ROS) and pertinent past, family and/or social history (PFSH).
Elements of History
Each type of history includes some or all of the following elements: CC, HPI, ROS and PFSH.
Chief Complaint: The patient encounter must include documentation of a clearly defined CC. Although it may be separate from the HPI and the review of systems, it must make the reason for the visit obvious, because it is the patient’s presenting problem. “Follow-up” does not constitute a chief complaint. A chief complaint should comprise a concise statement describing the symptom, problem, condition, diagnosis, physician-recommended return or other factors that establish the reason for the encounter in the patient’s own words (e.g., aching joints, rheumatoid arthritis, gout, fatigue, etc.). If a clear CC is not documented, the provider may be subject to a denial in the event of an audit and is usually referenced as not being medically necessity.
History of Present Illness: The HPI is a chronological description of the patient’s symptoms or clinical problems from the onset and/or how it has developed. HPI includes information obtained from the patient and must be obtained by the provider or a qualified healthcare professional. Some Medicare carriers have established their own policies that require the provider to perform the work of the HPI. Although interpretations of these policies may differ, the ACR recommends that practices review their contractor policies to avoid scrutiny.
HPI includes the following elements, in accordance with the 1995 documentation guidelines:
- Location—An area of the body, such as lower right leg, or the site of a problem or symptom, such as a sore throat.
- Duration—The length of time the patient has had the symptom or problem. Examples could include since last week, past three days, three years or last night.
- Severity—The intensity, degree or measure of the symptom or condition. Examples could include the worst pain I’ve ever experienced, pain is 5 on a scale from 1 to 10, not bad or severe.
- Quality—Describe the character or attribute of the symptom or condition. The descriptions can be defined as sharp, dull, throbbing, stabbing, scratchy, etc.
- Context—Surrounding events or what the patient was doing at the time the symptom or problem began. Examples could include falling going up the stairs or left tibia fractured while playing tennis.
- Modifying factor—What the patient has done to alleviate or try to fix the symptoms. Examples could include the patient took ibuprofen, applied an ice pack or used cortisone cream.
- Associated signs and symptoms—Document any additional signs associated with the primary problem, such as indigestion, chest pain, weakness or headache.
- Timing—Document when the symptoms began or occur. Examples could include every three hours, worse at night, hurts all the time or experiences pain every 30 minutes.
Two types of HPI—brief and extended—are distinguished by the amount of detail required to accurately characterize the clinical problem(s). A brief HPI consists of one to three elements, for example: Patient presents with pain in right toe [location] with swelling and burning [quality]—meets two HPI elements.
An extended HPI consists of four or more elements, for example: Patient presents with pain in right toe ([location] with swelling and burning [quality], and pain is a 9 out of 10 [severity]. Patient stated that she took an over-the-counter NSAID [modifying factor] and that the pain gets worse at night [timing]—meets five HPI elements.
In the 1997 guidelines, an alternate documentation requirement redefined the extended HPI for providers to list four or more elements of the HPI, or the status of three or more chronic or inactive conditions. But failure to document the status will negate the opportunity for the physician to receive HPI credit. Instead, this will allow the provider to receive credit only for a past medical history.
Review of System: The ROS consists of a series of questions used to elicit information about additional signs, symptoms or problems currently or previously experienced by the patient. The ROS may be recorded by someone other than the provider, but it is recommended that the provider make reference to the information in their own notes.
There are three types of ROS: problem pertinent, extended and complete, with 14 individual systems recognized by the E/M guidelines:
- Constitutional symptoms (e.g., fever, weight loss);
- Eyes;
- Ears, nose, mouth, throat;
- Cardiovascular;
- Respiratory;
- Gastrointestinal;
- Genitourinary;
- Musculoskeletal;
- Integumentary (skin and/or breast);
- Neurological;
- Psychiatric;
- Endocrine;
- Hematologic/lymphatic; and
- Allergic/immunologic.
A problem-pertinent ROS should be directly related to the problem listed in the HPI. For example, positive for pain in right toe; denies rashes, sprain, strain or fractures.
An extended ROS should relate directly to the HPI and some additional systems (2–9). For example, if there are two systems reviewed: patient denies chest pain, syncope, palpitations and shortness of breath. Patient indicates worsening unilateral pain in right toe.
Finally, a complete ROS should be directly related to a problem in the HPI, plus all additional organ systems (minimum of 10). All 10 systems must be individually documented with a positive or pertinent negative response. The remaining systems can be notated as “all other systems are negative,” if that is the case. For example, the following 10 signs and symptoms to record could include:
- Constitutional: weight stable, fatigue.
- Eyes: loss of peripheral vision.
- Ear, nose, mouth, throat: no complaints.
- Cardiovascular: denies palpitations; denies chest pain; denies calf pain, pressure, or edema.
- Respiratory: shortness of breath on exertion.
- Gastrointestinal: appetite good, denies heartburn and indigestion, no episodes of nausea. Bowel movement daily; denies constipation or loose stools.
- Urinary: denies incontinence, frequency, urgency, pain or discomfort.
- Skin: clammy, moist skin.
- Neurological: no fainting; denies numbness, tingling and tremors.
- Psychiatric: denies memory loss or depression, mood pleasant.
Past, Family and/or Social History: The last section of the history component includes the PFSH. For a new patient, all three elements must be documented, while established patients require only two of the elements for the highest level of PFSH. Providers do not have to duplicate a PFSH if there is an earlier version available on the chart. It is acceptable to review the earlier version of the PFSH and document any changes. In order to use this shortcut, you must record the date and location of the earlier version of the PFSH, but record any changes within the body of the current note.
The key purpose of complete & accurate documentation in the medical record is to foster a culture of quality & continuity of patient care.
The three areas of the PFSH for documentation include:
- Past history—experiences with illnesses, operations, injuries, and treatments;
- Family history—a review of medical events, diseases and hereditary conditions that may place the patient at risk; and
- Social history—age-appropriate review of past and current activities.
The two types of PFSH in the history component are pertinent and complete. A pertinent PFSH must have at least one area documented and be directly related to the problem in the HPI. A complete PFSH consists of two or all three areas (depending on the category of E/M service).
The key purpose of complete and accurate documentation in the medical record is to foster a culture of quality and continuity of patient care. Complete and accurate documentation creates thorough communication among providers, their staff and, ultimately, the patient for preventive health services, treatment, planning and delivery of care. When evaluating documentation for the history component of an E/M service, it is important to remember:
- A chief complaint is a medically necessary reason for the patient to be in the office. An identifiable CC is the first step in establishing medical necessity. A visit may be denied in an audit without a CC.
- If documentation substantiates that the provider is unable to obtain a history from the patient or other source (e.g., the patient is unconscious), the provider will not be penalized, and the overall level of medical necessity and/or provider work will not be discounted automatically.
- In the event that additional history is provided by a family member or caregiver and documented by the provider, it can be credited toward the medical decision-making component of the service.
- Past family and social history documented from a previous encounter may be cited without redocumentation for most payers. The provider should indicate the new status of the history and note where the original documentation may be found.
Although there are many nuances to the elements of the HPI component, understanding how to correctly document the patient’s history will put you on the right path to attain the correct coding level for each patient encounter. Documentation must reflect medical necessity for services to support the level of coding.
For questions or additional information on coding and documentation guidelines, contact Melesia Tillman, CPC‑I, CPC, CRHC, CHA, at 404-633-3777 x820 or via email at [email protected].
Reference
- Department of Health & Human Services. Centers for Medicare & Medicaid Services. Evaluation and Management Services (ICN 006764). 2016 Aug.
Editor’s note: In June on the Practice Page, we ran part 1 of a series, “Medical Decision Making Component.” Look for part 2 in the September issue.