Has your practice ever experienced the disappointment of being downcoded because of lack of supporting documentation?
Infusion services can be an important adjunct to treating patients with rheumatoid arthritis, ankylosing spondylitis, and other chronic diseases, and documenting time is a large part of showing the medical necessity of coding and billing for these services.
When there is no supporting documentation for infusion services, payers will deny or downcode claims as not medically necessary.
Starting this type of a service in an office-based practice can be a valuable tool in the spectrum of care for these chronically ill patients and can also provide an opportunity to become involved in clinical trials of infusion medications, thus offering patients a choice in participating in therapy that may otherwise not be available to them.
The importance of documenting time cannot be stressed enough. The reportable time that must be used to determine what codes can be billed, and whether add-on codes can be used, is the actual infusion time only. The preparation time, patient assessment time, time spent flushing the port in between subsequent infusions, post-service monitoring, and patient time in the waiting room cannot be counted towards billable infusion time.
There seems to be a great deal of confusion about when to start the time for intravenous infusions. The group of infusion codes that rheumatologists would use are:
- 96360: Intravenous infusion, hydration, initial, 31 minutes to one hour
- 96361: Each additional hour (List separately in addition to code for primary procedure)
- 96365: Intravenous infusion, for therapy, prophylaxis, or diagnosis (specify substance or drug); up to one hour
- 96366: Each additional hour (List separately in addition to code for primary procedure)
- 96413: Chemotherapy administration, intravenous infusion technique; up to one hour, single or initial substance/drug
- 96415: Each additional hour (list separately in addition to code for primary procedure)
The first qualifying initial hour must be at least 15 minutes and is coded as 96413. If it is less than 15 minutes, it should be coded as an intravenous push. This is coded as 96374. Physicians or their staff may report the infusion code for “each additional hour” only if the infusion interval time is greater than 30 minutes beyond the one hour increment.
For example, if the patient receives an infusion of a single drug that lasts one hour and 31 minutes, the physician would report the “initial” code of 96413 up to one hour and the add-on code of 96415 for the additional 31 minutes.
As you can see from the description of the codes, it is extremely important to accurately record the starting and stopping time of an infusion. The infusion time does not start until the infused medication begins to run through the IV. In the same manner, the stop time should be recorded when the infused medication is finished. Keep in mind, infusion time should not be estimated or started from the insertion of the IV port.
Accurate documentation of the start and stop time for infusions helps to support the medical necessity of these codes. Not understanding the guidelines can put your practice at risk for audits.
If you have any questions or concerns about this matter, contact the ACR’s coding and reimbursement specialist Melesia Tillman, CPC, CRHC, at (404) 633-3777, ext. 820, or at [email protected].
RhuemPAC Advancing Rheumatology Issues on Capitol Hill
RheumPAC, the ACR’s political action committee, ensures that the ACR is involved in healthcare reform discussions. RheumPAC representatives have been busy attending fundraisers and educating key congressional members on the ACR’s legislative priorities.
Sen. Lisa Murkowski (R-Ark.): RheumPAC attended a breakfast event for Sen. Murkowski, who is a member of the Health, Education, Labor, and Pensions co
Sen. Ron Wyden (D-Ore.): RheumPAC attended an event for Sen. Wyden to thank the senator for his support and discuss issues of importance to rheumatology health professionals regarding healthcare reform. Sen. Wyden is a member of the Senate Finance Committee and a co-sponsor of the “Medicare Fracture Prevention a
mmittee and a previous co-sponsor of the “Arthritis Prevention, Control, and Cure Act.” While at the event, RheumPAC representatives spoke with Sen. Murkowski about the importance of the pediatric loan repayment program and the provision to increase DXA reimbursement, and urged her to support keeping both provisions in the final Senate healthcare bill. nd Osteoporosis Testing Act.”
Rep. Frank Pallone (D-N.J.): Rep. Pallone is chair of the House Energy and Commerce Committee’s Subcommittee on Health, which has jurisdiction over various healthcare issues. RheumPAC attended an event for Rep. Pallone and had the chance to thank him for his support of the rheumatology community.
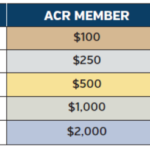
RheumPAC is the voluntary, nonpartisan political action committee of the ACR. It is the only PAC that directly represents the interests of rheumatology professionals on Capitol Hill. RheumPAC works to support and elect pro-rheumatology candidates.
Visit www.rheumatology.org/rheumpac or contact Katie Jones at [email protected] for more information on RheumPAC’s work.