
Rheumatology healthcare professionals have all seen postgastric bypass arthritis syndromes, but what if your patient had a gastric bypass after they were diagnosed with rheumatoid arthritis (RA)? Should these patients be treated differently?
Morbid obesity is fast becoming the most common co-morbidity associated with many types of arthritis. One-third of the U.S. population has a body mass index of greater than or equal to 30 kg/m2.1 Two hundred thousand gastric bypass surgeries are performed annually in the U.S.2
Rheumatology professionals spend much of our day counseling these individuals about diet, exercise and weight loss. We recognize that inflammatory arthritis and obesity further increase the mortality risk from cardiovascular disease in our patients. In addition, obesity may contribute to the development of RA or increase its severity due to the production of proinflammatory cytokines, such as TNF-α, IL-6, leptin, hepcidin and the siderophore, lipocalin-2, and may down-regulate the synthesis and secretion of antiinflammatory adipokines, particularly adiponectin.3,4 Thus, the adipose tissue functions as an organ, leading to a chronic, low-grade inflammatory state, which disturbs the absorption and metabolism of certain nutrients.
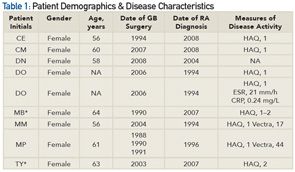
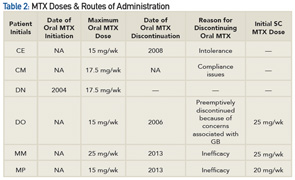
*Patients were ineligible for or were required to discontinue MTX because of suspected liver disease and were, therefore, excluded from the analysis.
Medication Absorption Post Gastric Surgery
Patients who are obese and have a diagnosis of RA who seek gastric bypass as a weight loss option require careful medication selection. Data demonstrate that changes in the physiology of the gut in gastric bypass patients result in malabsorption of many nutrients, such as vitamins A, B12, folate, D, calcium, E, K, zinc, iron and protein.5 Roux en Y procedures, the most common procedure performed in the U.S., is considered both a restrictive and malabsorptive procedure. This surgery reduces the size of the stomach to approximately 15–50 mL, decreasing its absorptive surface.6 Thus, patients undergoing this procedure may experience alterations in medication absorption, such as immunosuppressive drugs. Although there are no well-controlled randomized trials supporting this statement, data from case reports and case series suggest the absorption, first-line metabolism, volume of distribution and half-life of drugs may be substantially altered following bariatric surgery.7 The effects of these changes are drug dependent.
For example, Chenhsu et al described the need to double the dose of cyclosporine to achieve therapeutic levels in a patient with decompensated cirrhosis as a complication of jejunoileal bypass who subsequently underwent liver transplant.8 In patients who have had gastric bypass surgery, the route of administration of methotrexate (MTX) may need special consideration.
In a retrospective analysis of eight of our rheumatology patients who underwent gastric bypass via the Roux en Y procedure, we found that patients who could tolerate MTX did better switching to injectable MTX. Nonetheless, all eight patients were started on a biologic agent. The question arises: Would the patients have needed to be advanced to biologic therapy if they had been tried on parenteral MTX first (see Tables 1 and 2)?
Subcutaneous MTX
In one recent study, Schiff et al suggested subcutaneous (SC) MTX may be most effective in patients receiving oral MTX who are experiencing an inadequate clinical response.9 In this phase 2 study examining the effectiveness of SC MTX vs. oral MTX, the researchers reported that the dose of the oral MTX reached a plateau at 15 mg, whereas there was no plateau with the SC MTX. Thus, SC MTX provided higher systemic exposure to MTX than comparable oral doses. Relative bioavailability, as measured by area under the curve (AUC) of SC MTX vs. oral MTX at doses of 10, 15, 20 and 25 mg, was 121%, 114%, 131% and 141%, respectively. The ratio of the dose-normalized AUC (0–24 h) and Cmax of SC MTX vs. oral MTX were 127.61 (90% CI: 122.30–133.15) and 94.88 (90% CI: 87.95–102.37). These observations appear to be consistent with the clinical experience of many practitioners who have noted a benefit to using parenteral rather than oral MTX.
Rheumatology is fast becoming a specialty of complex immunology and targeted genetic therapies. To best serve our patients, rheumatology health professionals should carefully scrutinize all treatment modalities and drug bioavailabilities, especially among those patients who have undergone gastric bypass surgery.

Iris Zink, NP, has worked in the Rheumatology Department at the Beals Institute in Lansing, Mich., for 15 years. She is the president elect of the Rheumatology Nurses Society and co-authored the chapter in the Rheumatology Nurses Society core curriculum on HIV and arthritis. She is also adjunct faculty at Michigan State University.
References
- Ogden CL, Carroll MD, Flegal KM. Epidemiologic trends in overweight and obesity. Endocrinol Metab Clin North Am. 2003;32:741–760.
- American Society for Metabolic and Bariatric Surgery. asmbs.org.
- Puglisi MJ, Fernandez ML. Modulation of C-reactive protein, tumor necrosis factor-alpha, and adiponectin by diet, exercise, and weight loss. J Nutr. 2008; 138(12):2293–2296.
- O’Rourke RW. Inflammation in obesity-related diseases. Surgery. 2009;145:255–259.
- Xanthakosa SA, Thomas IH. Nutritional consequences of bariatric surgery. Curr Opin Clin Nutr Metab Care. 2006;9:489–496.
- Sawaya RA, Jaffe J, Friedenberg L, Friedenberg FK. Vitamin, mineral, and drug absorption following bariatric surgery. Curr Drug Metab. 2012;13(9):1345–1355.
- Malone M. Altered drug disposition in obesity and after bariatric surgery. Nutr Clin Pract. 2003;18(2):131–135.
- Chenhsu RY, Wu Y, Katz D, Rayhill S. Dose-adjusted cyclosporine c2 in a patient with jejunoileal bypass as compared to seven other liver transplant recipients. Ther Drug Monit. 2003;25:665–670.
- Schiff MH, et al. Head-to-head, randomised, crossover study of oral versus subcutaneous methotrexate in patients with rheumatoid arthritis: Drug-exposure limitations of oral methotrexate at doses ≥15 mg may be overcome with subcutaneous administration. Ann Rheum Dis. 2014;73(8):1549–1551.
