optimarc / shutterstock.com
CHICAGO—John H. Stone, MD, MPH, director of clinical rheumatology at Massachusetts General Hospital, Boston, took the stage at the 2018 ACR/ARHP Annual Meeting to present, for the first time, a draft of new classification criteria for IgG4-related disease (IgG4-RD), a project supported by both the ACR and EULAR. Even though it was the last day of the meeting, the room was full, and Dr. Stone commented it was extraordinary to have so many people come together to learn about IgG4-RD.
“Fifteen years ago the existence of the disease was only beginning to dawn on us,” said Dr. Stone. “Now it is clear that IgG4-RD is really a global disease, and it is high time we understood how to classify patients who might have this condition; what is IgG4-RD, and what is not? The past 15 years with this condition tell a fascinating story.” He added, “IgG4-RD is a perfect disease for rheumatologists.”
Classification Criteria Development
Patients with IgG4-RD tend to present with symptoms for months or years before diagnosis. Fevers are unusual, erythrocyte sedimentation rate/C-reactive protein dissociation is common, and weight loss can be prominent.
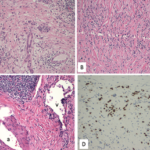
IgG4-RD is often mistaken for a malignancy—pancreatic cancer, lymphoma, multiple myeloma and others—and this is one reason pathologists were the first, in the early days of identifying the disease, to make the diagnosis. Pathologists received surgical resection samples from patients who were believed to have cancer. On closer inspection, they realized the patients did not have cancer, but rather had an inflammatory and fibrotic disorder with a tendency to form mass lesions that mimicked cancer.
Although IgG4-RD is noteworthy for its histopathology and immunostaining findings that are consistent across all organs, these pathology findings cannot be truly diagnostic of this disease without also assessing information from the clinical presentation, serological findings and radiology studies. The need to triangulate among different sources of data is the essence of the approach to IgG4-RD classification criteria development.
The draft IgG4-RD classification criteria target a specificity of >90% and a sensitivity of >80%. The criteria were developed by a working group that included 79 members from the U.S., Europe, Japan and elsewhere. The members focused on developing criteria that would prevent patients who do not have IgG4-RD from being inappropriately enrolled in clinical trials and at the same time not exclude too many with atypical presentations of IgG4-RD.
Inclusion & Exclusion Factors
The working group developed the criteria on the basis of 487 cases and mimickers, and tested the criteria on an additional 908 cases and mimickers. The group determined that classification required the involvement of at least one organ from a list of 10: pancreas, bile ducts, orbits, lacrimal glands, major salivary glands, retroperitoneum, kidney, aorta, pachymeninges and thyroid gland (Riedel’s thyroiditis, but not Hashimoto’s disease). They specifically excluded patients with fevers, those who failed to respond to steroids, those with leukopenia and thrombocytopenia, as well as those with extreme peripheral eosinophilia. They also excluded patients who were positive for anti-neutrophil cytoplasmic antibodies, antibodies to the Ro antigen and autoantibodies specific to other diseases.
The working group noted that although radiology is less helpful than clinical, serological and pathological data, rapid radiological progression of a lesion argues strongly against IgG4-RD. Finally, because malignant infiltration and necrotizing vasculitis are more common in mimickers than in IgG4-RD, they excluded patients who met these criteria.
The group found the clinical exclusion criteria were successful in eliminating 31% of mimickers. A larger percentage (42%) were excluded by the serological criteria, meaning they were positive for anti-neutrophil cytoplasmic antibodies (ANCA), anti-Ro/SSA and/or anti-La/SSB antibodies. Approximately 10% of patients failed the radiological exclusion criteria, and 42% failed the pathological exclusion criteria. Dr. Stone noted some patients failed more than one category of exclusion criteria.
The classification criteria also include eight weighted inclusion criteria. Patients, for example, scored inclusion points in the serum IgG4 domain based on how high their IgG4 levels were. In addition, an uninformative biopsy was worth zero points, but other observations gave more points. With kidneys, for example, maximum points were given for renal pelvis thickening and fewer points for hypocomplementemia. Patients received maximum points for the presence of circumferential or anterolateral soft tissue around the renal aorta or iliac arteries. Dr. Stone emphasized this radiologic pattern in the kidneys makes him highly suspicious of IgG4-RD.