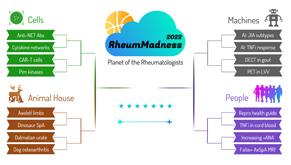
 Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The more your picks match those of our Blue Ribbon Panel of rheumatologists, the more points you get. Learn more about the panel and how the brackets work online.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn more on the RheumMadness website.
Region: People Team: TNFi in Cord Blood
Wardell Stephen “Dell” Curry Sr. and Steph Curry, Tim Hardaway and Tim Jr., Joe and Kobe Bryant—all exemplify athletic skill passed from parent to child. In this scouting report, we explore a different type of transference to help patients and providers understand the safety of tumor necrosis factor (TNF) inhibitor use during pregnancy.
 The 2016 EULAR Points to Consider for Use of Anti-Rheumatic Drugs Before Pregnancy, and During Pregnancy and Lactation support the use of TNF inhibitors during the first half of pregnancy.1 Although the EULAR taskforce synthesized existing data to develop much-needed recommendations, the analysis was limited by the need to focus on widely studied end points, such as congenital malformations. Quantifying drug levels transferred to the fetus during pregnancy would be the most useful. But how could this be done safely given the vulnerable population being studied?
The 2016 EULAR Points to Consider for Use of Anti-Rheumatic Drugs Before Pregnancy, and During Pregnancy and Lactation support the use of TNF inhibitors during the first half of pregnancy.1 Although the EULAR taskforce synthesized existing data to develop much-needed recommendations, the analysis was limited by the need to focus on widely studied end points, such as congenital malformations. Quantifying drug levels transferred to the fetus during pregnancy would be the most useful. But how could this be done safely given the vulnerable population being studied?
That’s where our article comes in. Our base article is one of the few larger trials looking at biochemical evidence of TNF inhibitor concentrations in cord blood, thus helping quantify drug transference from mother to fetus during pregnancy.2 In the study, all anti-TNF drugs were stopped at the time recommended by EULAR (typically between 20 and 37 weeks of gestation).1 Results showed that adalimumab (n=25; stopped by week 20) was detected in 48% of cord blood samples; infliximab (n=14; stopped by week 20) was detected in 57% of cord blood samples; certolizumab (n=68; continued throughout pregnancy) was detected in 5.9% of cord blood samples; and etanercept (n=30; stopped prior to week 30) was not detected in any cold blood samples (lower limit of quantification 0.1 μg/mL).
The observation that detectable drug concentrations were measured in many of the samples is reason to pause and ask: What is the clinical significance of this finding?
The concentration ratio of TNF inhibitors in cord blood to maternal blood ranged from 0.01 to 0.062, depending on the agent, suggesting very low levels of transfer. The clinical significance of these levels of anti-TNF agents may not be fully established, but we have plenty of evidence to suggest the levels are safe. Studies have shown concentrations of 0.1 μg/mL can bind all circulating TNF, suggesting this level as a cutoff value for clinically relevant concentrations.3
Infants born to mothers on anti-TNF therapy have been studied more extensively in inflammatory bowel disease (IBD) literature. Those studies have shown the use of biologic therapy during pregnancy does not affect infant response to vaccines or achievement of developmental milestones, or increase the risk of infection.4-6
Certolizumab is the anti-TNF treatment we all know and love because it’s safe during pregnancy. It’s known for its unique lack of immunoglobulin G (IgG) fragment crystallizable (Fc) region, which keeps it from binding to the placental Fc receptor and, thus, is not transferred across the placenta from mother to fetus.7 But what about etanercept? Previous studies suggest some transplacental transport via antibody Fc fragment, but our base article suggests a lack of significant placental transfer.8 Along with evidence suggesting little, if any, placental transfer during pregnancy when stopped prior to 30 weeks of gestation, this finding may elicit a stronger support for use of etanercept throughout pregnancy.
The ACR guideline is notably less specific than EULAR, grouping most TNF inhibitors—other than certolizumab—together into the same category, with the conditional recommendation to continue these treatments during the first and second trimesters and discontinue during the third trimester, several half-lives prior to delivery.9 Guidelines for pregnant patients with IBD on biologic therapy recommend continuing biologics throughout pregnancy without interruption.10 Instead of discontinuing therapy, providers typically adjust the final dosing prior to delivery to achieve a low estimated trough because this is associated with lower adverse pregnancy outcomes for both mother and baby.
Implications
The implications of this study for patients cannot be overstated. In this unique circumstance, in which providers are taking care of both the mother and baby, every decision matters. These results can help providers make specific, patient-centered recommendations for their patients when it comes to the use of TNF inhibitors during pregnancy. The methods used in this study serve as an example of how to further examine transference of biologics and other drugs from mother to fetus.
Although guidelines are a great resource for all patients and providers, this study gives us more detailed information to make specific and patient-centered decisions.
Chances in the Tournament
TNFi in Cord Blood takes medication management in pregnancy one step further by looking at the science behind the guidelines and even rocks the boat on some current recommendations. Additionally, it gives us biochemical evidence supporting their safe use during pregnancy.
Our article creates an excellent base for further research on the topic of safe medications during pregnancy and continuously improving recommendations for our patients, both large and small.
Lauren He, MD, is an internal medicine resident at University of Chicago Medicine.
Cuoghi Edens, MD, is an assistant professor of Internal Medicine & Pediatrics, Section of Rheumatology & Pediatric Rheumatology at University of Chicago Medicine.
References
- Gotestam Skorpen C, Hoeltzenbein M, Tincani A, et al. The EULAR points to consider for use of antirheumatic drugs before pregnancy, and during pregnancy and lactation. Ann Rheum Dis. 2016 May;75(5):795–810.
- Ghalandari N, Kemper E, Crijns I. Analysing cord blood levels of TNF inhibitors to validate the EULAR points to consider for TNF inhibitor use during pregnancy. Ann Rheum Dis. 2021 Sep 7;annrheumdis-2021-221036.
- Berkhout LC, I’Ami MJ, Ruwaard J, et al. Dynamics of circulating TNF during adalimumab treatment using a drug-tolerant TNF assay. Sci Transl Med. 2019 Jan 30;11(477):eaat3356.
- Beaulieu DB, Ananthakrishnan AN, Martin C, et al. Use of biologic therapy by pregnant women with inflammatory bowel disease does not affect infant response to vaccines. Clin Gastroenterol Hepatol. 2018 Jan;16(1):99–105.
- De Lorenzo R, Ramirez GA, Punzo D, et al. Neonatal outcomes of children born to mothers on biological agents during pregnancy: State of the art and perspectives. Pharmacol Res. 2020 Feb;152:104583.
- Tsao NW, Lynd LD, Sayre EC, et al. Use of biologics during pregnancy and risk of serious infections in the mother and baby: A Canadian population-based cohort study. BMJ Open. 2019 Feb 20;9(2):e023714.
- Mariette X, Froger F, Abraham B, et al. Lack of placental transfer of certolizumab pegol during pregnancy: Results from CRIB, a prospective, postmarketing, pharmacokinetic study. Ann Rheum Dis. 2018 Feb;77(2):228–233.
- Berthelsen BG, Fjeldsøe-Nielsen H, Nielsen CT, et al. Etanercept concentrations in maternal serum, umbilical cord serum, breast milk and child serum during breastfeeding. Rheumatology (Oxford). 2010 Nov;49(11):2225–2227.
- Sammaritano LR, Bermas BL, Chakravarty EE, et al. 2020 American College of Rheumatology guideline for the management of reproductive health in rheumatic and musculoskeletal diseases. Arthritis Rheumatol. 2020 Apr;72(4):529–556.
- Mahadevan U, Robinson C, Bernasko N, et al. Inflammatory bowel disease in pregnancy clinical care pathway: A report from the American Gastroenterological Association IBD Parenthood Project Working Group. Gastroenterology. 2019 Apr;156(5):1508–1524.
 Experience All of RheumMadness
Experience All of RheumMadness
During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports. Check out the reports from each region:
Region: Cells
Region: Animal House
Region: Machines
Region: People
• False Positive MRI in Axial SpA
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The winner of each match-up is decided by a seven-member Blue Ribbon Panel of rheumatologists. The panel will vote based on which topic they think is most important to patients, providers and researchers—both now and in the future. The more your picks match those of the panel, the more points you get. The tournament results will be released in four rounds from March 26–April 4. Prizes will be given to participants with the top scores in the following categories: 1) attending/APP, 2) fellow and 3) resident/medical student. The prize is a custom RheumMadness coffee mug and a lifetime of bragging rights.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn on the RheumMadness website.



