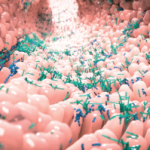
The healthy human intestinal microbiome is characterized by a balance between niche diversity and a relative abundance of members of the Bacteroidetes and Firmicutes phyla. Increasingly, research has revealed that this balance influences health and disease, and recently, evidence has accumulated to suggest that the microbiome may also play a role in tissue-specific autoimmunity. This year, Sjögren’s syndrome was added to the list of autoimmune conditions that are associated with intestinal dysbiosis. Specifically, researchers have revealed that patients with Sjögren’s syndrome have a dysbiotic intestinal microbiome that is characterized by a low relative abundance of commensal bacteria and a high relative abundance of potentially pathogenic genera. This dysbiosis is associated with worse ocular mucosal disease in patients with Sjögren’s syndrome, as well as a mouse model of Sjögren’s syndrome.
The healthy human intestinal microbiome is characterized by a balance between niche diversity and a relative abundance of members of the Bacteroidetes and Firmicutes phyla. Increasingly, research has revealed that this balance influences health and disease, and recently, evidence has accumulated to suggest that the microbiome may also play a role in tissue-specific autoimmunity. This year, Sjögren’s syndrome was added to the list of autoimmune conditions that are associated with intestinal dysbiosis. Specifically, researchers have revealed that patients with Sjögren’s syndrome have a dysbiotic intestinal microbiome that is characterized by a low relative abundance of commensal bacteria and a high relative abundance of potentially pathogenic genera. This dysbiosis is associated with worse ocular mucosal disease in patients with Sjögren’s syndrome, as well as a mouse model of Sjögren’s syndrome.
Cintia S. de Pavia, MD, PhD, assistant professor of ophthalmology at Baylor College of Medicine in Houston, and colleagues published the results of their microbiome analysis online on April 18 in Scientific Reports. They began their investigation in a validated mouse dry eye model with features of Sjögren’s syndrome. The mice were exposed to a desiccating stress (DS) environment, and the researchers measured the effect of DS on the intestinal microbiome of the mice. They compared those results with those of mice that received a cocktail of oral antibiotics for 14 days prior to and during exposure to DS. The investigators found that mice that received antibiotic treatment plus DS had less microbiome diversity than did mice that received DS alone. Additionally, the mice in the antibiotics-plus-DS group had greater goblet cell loss and an increased number of CD4+ T cells infiltrating the conjunctival epithelium than did mice that received DS alone. The researchers concluded from their results that although DS stress alone could cause a significant increase in Proteobacteria, oral antibiotics plus DS resulted in extreme changes in the gut microbiota.
Based on these mouse data, the investigators initiated a pilot study comparing the microbiome of the conjunctiva, tongue and stool of patients with Sjögren’s syndrome to the microbiome of healthy control subjects. They found that the stool from patients with Sjögren’s syndrome had greater relative abundances of Pseudobutyrivibrio, Escheria/Shigella, Blautia and Streptococcus and a lesser abundance of Bacteroides, Parabacteroides, Faecalibacterium and Prevotella relative to controls. Although the investigators found differences between the control and Sjögren’s syndrome groups in the stool and tongue microbiome, they found no differences in the conjunctival microbiome.
“In this pilot study, we observed distinct differences in the oral and stool microbiome in the Sjögren’s syndrome group compared [with] controls, characterized by a decreased microbial richness in the mouth and significant differences in certain genera in both mucosal sites,” write the authors in their discussion. “Subjects with the most severe keratoconjunctivitis sicca and combined systemic and ocular disease were found to have the lowest diversity of stool microbiota. It remains to be determined if the observed changes in the mucosal microbiome result from the secretory glandular dysfunction, defective cholinergic signaling with altered gastrointestinal motility, or mucosal disease in Sjögren’s syndrome and/or if the mucosal dysbiosis is a stimulus for development or exacerbation of the autoimmune mucosal and glandular disease immunopathology at these sites.”
Lara C. Pullen, PhD, is a medical writer based in the Chicago area.
References
- Cintia S. de Paiva, Dan B. Jones, Michael E. Stern, et al. Altered mucosal microbiome diversity and disease severity in Sjögren’s syndrome. Sci Rep. 2016; 6:23561. Published online 2016 Apr 18. doi: 10.1038/srep23561.