Pathogenesis & Clinical/Laboratory Features
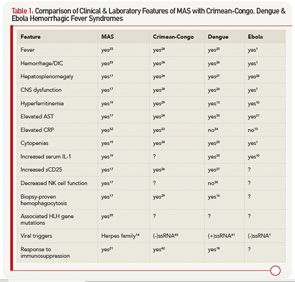
Following the transmission of Ebola virus, studies in NHPs indicate the virus initially infects differentiated dendritic cells and macrophages.5 Initial clinical manifestations in infected individuals who become symptomatic are nonspecific, with fever, headache, myalgia and enteritis, appearing anywhere between two and 21 days.6 With progression to stages of greater severity, Ebola virus is subsequently detected in endothelial cells, hepatocytes and other tissues, with clinical and laboratory features that are very similar to what is observed in other hemorrhagic fever viruses (see Table 1).7 Liver dysfunction, including AST and ALT elevations, is quite frequent and may be accompanied by jaundice. Although leukocytosis may occur early, this is frequently followed by the development of significant lymphopenia and neutropenia. Profound coagulopathy with hypofibrinogenemia, d-dimer elevations, LDH elevations and thrombocytopenia develop as preterminal events in association with mucosal hemorrhage and multi-organ failure.
Host Immunologic Response
Within hours of Ebola binding to macrophages, even prior to evidence of viral replication, there is significant macrophage activation and release of proinflammatory cytokines.8,9 These in vitro observations correlate with significant measured serum elevations in macrophage-derived cytokines, including IL-1β, TNF, IL-6, IL-15, IL-16 and IL-8, as well as chemokines, including MIP-1, MCP-1, M-CSF and IP-10, that are observed during the early stages of infection.10 Although mRNA expression studies confirm evidence of eventual T cell activation, elevations in cytokines specific to T cell activation, such as IL-12 or IL-17, are typically not observed in the early stages of infection. Noteworthy is the apparent suppression of interferon responses that is mediated by two viral proteins, VP24, which blocks nuclear localization of interferon triggered transcription factors, and VP35, which inhibits or inactivates several type-I interferon regulatory factors (IRF-3, IRF-7).4 The ability of the virus to attenuate antiviral interferon responses may, therefore, contribute to the establishment and rapid dissemination of infection in the host.
It is instructive and important to recognize that while the symptomatic attack rate in Ebola virus is very high, not all individuals who acquire the virus develop symptoms.11 In prospective studies of family members having close contact with symptomatic Ebola virus disease patients, a number of individuals mount effective IgM and IgG responses to viral proteins in the context of confirmed viremia with genotype identical virus, yet do not develop symptoms. In these individuals, high levels of proinflammatory macrophage-derived cytokines, including IL-1β (see Table 1), TNF, IL-6, MCP and MIP-1α/β, are observed early, within five to seven days of the initial contact. However, this occurs in temporal association with a robust antiinflammatory response with measured high concentrations of IL-1Ra, sTNFRI/sTNFRII, IL-10 and cortisol, with rapid decline in the levels of the proinflammatory cytokines to normal two to three days after the initial rise. Although T cell-derived cytokines were not detected in the plasma of asymptomatic infected individuals, increased IL-2, IL-4, IL-12, IFNγ, Fas, FasL and perforin mRNA expression occurs and peaks nine to 16 days after exposure. These observations are consistent with the development of a cytotoxic CD8 T cell response required for the killing of Ebola-infected cells, as well as CD4 T helper cell responses that likely promote the noted rise in Ebola-specific IgG1 and IgG3 antibody levels.
