Methotrexate
lyricsaima / Shutterstock.com
MADRID—Tofacitinib (a JAK inhibitor) used with methotrexate (MTX) is not inferior to adalimumab (a TNF inhibitor) in rheumatoid arthritis (RA) patients who’ve had an inadequate response to MTX alone, according to results of a Phase 3B/4 trial presented in a session at the Annual European Congress of Rheumatology (EULAR).
The findings came in a one-year trial, called ORAL Strategy, with three active treatment arms, meant to compare tofacitinib alone with tofacitinib plus MTX, tofacinitib alone with adalimumab plus MTX, and tofacitinib plus MTX with adalimumab plus MTX (see Table 1).1
In the other comparisons, performed using an efficacy threshold derived from a meta-analysis of adalimumab trials, tofacitinib alone landed in a kind of statistical limbo when compared with adalimumab plus MTX: It wasn’t shown to be worse, nor was it shown to be superior. The same was found for tofacitinib alone compared with tofacitinib plus MTX. The main point of the trial was to settle remaining questions from tofacitinib’s Phase 3 trial, which suggested that perhaps tofacitinib alone was better than tofacitinib with MTX—which was found not to be true in this trial—and that tofacitinib with MTX was better than adalimumab.
The Trial
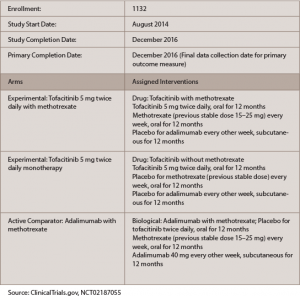
(click for larger image)
Table 1: ORAL Strategy
One thousand one hundred and forty-six patients were randomized: 384 were treated with 5 mg tofacitinib monotherapy orally twice a day, 5 mg tofacitinib twice a day plus MTX or adalimumab plus MTX.
There was no significant difference between the groups, with 46% of the tofacitinib-plus-MTX patients achieving an ACR50 response after six months, compared with 43.8% of adalimumab-plus-MTX patients and 38.3% of the tofacitinib-alone patients. In a subsequent analysis, tofacitinib plus MTX was not found to be superior to adalimumab plus MTX.
“In a group of patients, you can start [tofacitinib] or you can start adalimumab, and you can expect the same result with either,” said Roy Fleischmann, MD, clinical professor of internal medicine at University of Texas Southwestern Medical Center, who presented the results, recently published in The Lancet. He added, “Anyone who interpreted the Phase 3 studies showing that monotherapy [tofacitinib] looks better than the combination of tofacitinib plus MTX should correct their perception.” Monotherapy tofacitinib was found to be “not non-inferior” to tofacitinib plus MTX, landing in a kind of statistical middle ground in which non-inferiority wasn’t demonstrated, but neither was superiority.
The three groups had no major differences in the occurrence of adverse events, except that liver function was better in the tofacinitib-alone group—with at least 12% fewer patients having aspartate transaminase and alanine transaminase at the upper limit of normal or higher, compared with the other treatment groups.
“That’s one of the reasons why I like monotherapy tofacitinib; there’s less LFT [liver function test] elevation with the monotherapy than there is with combination, and LFT elevation concerns me when methotrexate is on board,” he said.
What This Means
Dr. Fleischmann said the results validate what is common treatment practice.
“[If] I have a patient who’s on methotrexate, [and] they have an incomplete response to methotrexate, I add tofacitinib. I don’t switch. I add,” he said. “And if the patient has a good response, a really good response, then I discontinue methotrexate. And what I see in practice is that about two-thirds or three-quarters of patients do well with tofacitinib monotherapy; there are, however, some patients who do better with combination of tofacitinib plus methotrexate.”
Dr. Fleischmann was asked how he would reconcile these results with findings, published earlier this year, that monotherapy with baricitinib, another JAK inhibitor, was superior to adalimumab plus MTX, even though tofacitinib was not found to be superior to adalimumab plus MTX in this trial.2
He said this trial should not call into question the baricitinib findings. “There would have to be a head-to-head trial of tofacitinib vs. baricitinib,” he said. “You can’t compare one trial with another in different study populations.”
RA Medication Study
In an 810-patient study, researchers found that those started on a higher dose of MTX, 15 mg or higher, were more likely to have a good response according to EULAR criteria than those started on a lower dose, 7.5 mg or lower.
It was an effort to get at the appropriate starting dose of the drug, a subject that is open to question, sometimes leading to varying treating patterns.
In the study, which used data from the U.K.’s 35-center Rheumatoid Arthritis Medication Study (RAMS), 171 patients were in the low-dose group and 639 in the high-dose group.3 Patients in the high-dose group had significantly lower Visual Analogue Scores (VAS) than the low-dose group (P=.0001) at baseline and were significantly less likely to be given concomitant non-biological disease-modifying drugs (P=.003), said Rebecca Davies, a research assistant at the University of Manchester, who presented the findings.
Those in the high-dose group were significantly more likely to have achieved a good EULAR response after six months, with a relative risk ratio of 2.65 (P=.004). She noted that the study looked only at the starting dose and didn’t take into account any escalations.
Dr. Fleischmann said the chosen “high” dose of 15 mg is actually fairly low and that 20 mg is a dose more commonly considered high, although a session moderator pointed out that some studies have found that, given orally, there is not much of an increase in the bioavailability of the drug at doses higher than 15 mg.
Ms. Davies said the study focused on the two most commonly prescribed doses in the U.K. and that these were the two most disparate doses that allowed a workable analysis. “It’s become more common in the U.K. in more recent years to prescribe a 10 mg dose,” she said, “and I’d like to repeat this analysis looking at that group of patients.”
Thomas R. Collins is a freelance writer living in South Florida.
References
- Fleischmann R, Mysler E, Hall S, et al. Efficacy and safety of tofacitinib monotherapy, tofacitinib with methotrexate, and adalimumab with methotrexate in patients with rheumatoid arthritis (ORAL Strategy): A phase 3B/4, double-blind, head-to-head, randomised controlled trial. Lancet. 2017 Jun 15. pii: S0140–6736(17)31618-5. [Epub ahead of print]
- Taylor P, Keystone E, van der Heijde D, et al. Baricitinib versus placebo or adalimumab in rheumatoid arthritis. N Engl J Med. 2017 Feb 16;376(7):652–662.
- Davies R, Lunt M, Barton A, et al. The effect of a low versus high first prescribed dose of methotrexate on EULAR response at six months using data from the RAMS study (abstract OP0225). Annual European Congress of Rheumatology. 2017 Jun 15. Madrid, Spain.

