Further analysis of the seasonality of Kawasaki disease and associated epidemics in Japan, Hawaii and San Diego suggests a relationship between seasonal and epidemic peaks and wind currents originating from central Asia and traveling through the North Pacific, with a very short lag time to disease onset, based on the temporal and spatial distribution of cases.9,10 The authors hypothesized a role for a windborne pathogen, such as a mycobacteria or a noninfectious toxin.
Infection & the Microbiome
Various infectious agents have been suggested to be a trigger for JIA, but few controlled studies exist (reviewed in references 11–13). Cyclical variations in the incidence of JIA in Manitoba, Canada, with three- to five-year peaks in the cycles, correlated with concomitant increases in Mycoplasma pneuomoniae infections.14 Parvovirus B19 has been associated with JIA, with an increased frequency of immunoglobulin (Ig) M and IgG antibodies against the organism and viral DNA in the serum and synovial fluid in JIA patients, compared with controls, but other studies have not confirmed this association.15,16
The role of infection early in life and increased exposure to infectious agents via larger family size, urban dwelling or contact with animals is part of the hygiene hypothesis, which posits that increased exposure to infection early in life may be protective for the development of autoimmune disease.13
Some well-designed studies do not support the hygiene hypothesis in JIA, however, with several large case-control studies based on medical record review and use of registry data concluding that an increase in early-life infections and antibiotic usage are risk factors for JIA.
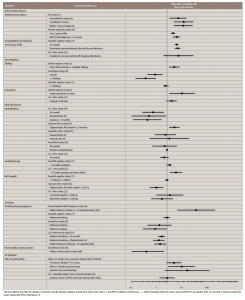
A large case-control study of electronic medical records from more than 550 general pediatric practices in the U.K. showed that antibiotic exposure is associated with development of JIA. They found that a higher risk of JIA was associated with more courses of antibiotic use, with the strongest effect within 12 months of diagnosis, even when adjusting for the number and type of infections (see Table 2). These findings suggest a potential role for bacterial infection or for an alteration of the microbiome in disease development.17
(click for larger image)
Table 2: Possible Environmental Risk Factors Associated with Juvenile Idiopathic Arthritis (JIA)*
*All associations are with JIA, except as noted for specific disease subtype. Forest plots show odds ratio ( • ) and 95% confidence interval (CI, — ). Risk is elevated when the mean value and 95% CI are greater than 1.0, and risk is reduced when the mean values and 95% CI lie below 1.0.


