Magnetic resonance imaging (MRI) provides a wonderful capacity for imaging all the tissues involved in rheumatoid arthritis (RA) and osteoarthritis (OA). For rheumatologists, MRI can be useful in both conditions.
MRI does not use ionizing radiation to produce its images, but instead depends on an external magnetic field, radiofrequency pulses, and the actions of hydrogen protons within a given region of interest. On T1-weighted images, bone has high signal intensity (white), while fat-suppressed or short T1 inversion recovery (STIR) images suppress the signal from bone marrow fat so that the only areas with high signal are those with increased water content, such as areas of inflammation. Contrast agents, such as gadolinium, enhance the MR signal in areas of high vascular flow or increased capillary permeability, and such paramagnetic agents are required for optimal detection of synovitis or tenosynovitis.
The majority of MRI scans are done using 1.5 Tesla (T) magnets, although 3T magnets are increasingly available. Usually, increased magnet strength results in improved resolution of images. However, the clinical gains of such increased resolution are offset against clinical issues of feasibility. In the last few years, more low field (<1T) magnets, called extremity (eMRI) machines have been used. These machines provide a much more patient-friendly imaging technique, because they only require insertion of a limb and reduce patient claustrophobia issues. Generally, the image quality is reduced compared with high-field MRI.
Not every patient can have an MRI scan. Metal under the skin can cause artifacts and there is obviously great danger if there are metal fragments in an eye. People with pacemakers should not go near magnetic fields. Occasionally, people may not fit in a large bore MRI machine due to obesity, and sometimes the receiver coil for a joint such as the knee will not fit around a very large knee.
MRI is dramatically increasing our understanding of structural pathology in arthritis.
RA Pathology on MRI
Erosions: The radiographic erosion is the hallmark of RA. The tomographic nature of MRI markedly improves the ability to detect erosions compared with traditional radiographs, even when using eMRI. Initial publications on this imaging modality described the validity of MRI erosions to predict subsequently visualized erosions on radiographs. Computed tomography (CT) is the gold standard for examining cortical bone, and recent studies have shown high correlations between MRI and CT detected erosions in RA, thereby validating that the MR erosions are the equivalent of radiographic erosions, with the increased detection rate reflecting the tomographic advantages of MRI.1,2
Synovitis and Tenosynovitis: Contrast-enhanced MRI shows inflammation and damage simultaneously. (See Figure 1, right.) Studies in the wrist and metacarpophalangeal joints have demonstrated that the volume of synovitis can predict subsequent erosion progression. MRI studies have demonstrated a clear relationship between inflammation and progression of bony damage at the individual joint level.3 Longitudinal studies of MRI tenosynovitis at the wrist have also demonstrated predictive validity for subsequent tendon rupture.
Bone Edema: Bone edema is one of the most interesting features to emerge from MRI studies. Radiologists first reported this feature in the late 1980s. The appearance can refer to a range of pathological processes, and is descriptive for high signal lesions in bone on fat-suppressed or STIR images. In RA, bone edema refers to a pathological process that spans the continuum from activity to damage. Early studies demonstrated that bone edema is proportional to the adjacent degree of synovitis; recent studies have confirmed that areas of edema represent an inflammatory cell infiltrate or osteitis.4 If this osteitis persists, then trabecular bone loss occurs and an erosion is formed. However, effective treatment can reduce the early bone edema lesion and thereby stop the erosion formation.
MRI in RA Research
MRI is ideal for studies on pathogenesis and therapeutic outcome because of its increased sensitivity for bony damage and ability to simultaneously visualize inflammation. Studies have demonstrated that imaging one wrist and four metacarpophalangeal (MCP) joints in a single hand is more sensitive (by a factor of 2.5) than bilateral hand and feet radiographs in detecting erosion progression over a 12-month period.5 Studying synovitis in RA trials generally requires intravenous contrast use and is often limited to studying either a single wrist or four MCP joints.
Quantification of MRI-detected RA pathology is continually improving. There are detailed volumetric methods for measuring erosion size and synovitis volume. Furthermore, dynamic contrast enhanced MRI can be used to assess synovitis, although generally it is limited to single site studies. One of the most commonly used MRI scoring systems is the RA MRI score developed by OMERACT, which is a semi-quantitative score evaluating synovitis, bone edema, and erosions. This score has been validated in a number of studies. Quantitative whole organ image analysis methods are under development and may be available within the next few years.
Until now, RA studies using MRI have been limited to a relatively small number of proof-of-concept or phase II studies. However a number of large randomized RA trials are currently employing MRI, which may eventually result in change of regulatory status.
MRI in RA Clinical Practice
MRI has been responsible for clarifying a number of concepts about RA. First, it has clarified the nature of the relationship between inflammation and damage. It has also helped us understand that subclinical synovitis (i.e., inflammation present in joints that are not detected clinically on joint examination) is common. In a cohort of over 100 patients with low disease activity, over 80% had synovitis when one hand was imaged by MRI.6 The presence of subclinical disease helps to explain the discrepancies when joints that have apparent clinical remission show ongoing radiographic destruction. Such inflammation will make us look harder at what we call “remission” and may lead to us to aim for imaging remission.
Apply caution when jumping from the concepts that MRI has provided to the routine use of MRI in the clinic. At present, there is little information to suggest that MRI is useful in the differential diagnosis for peripheral joints, and defined clinical algorithms are needed before routine use can be advocated. In terms of monitoring erosion progression, there may be a role for the added sensitivity of MRI, especially if it is linked to the better tolerated eMRI. Such use in routine practice would require that individual patient images are always evaluated alongside the previous MR examination, that is, the presence of a systematic longitudinal evaluation whether performed by rheumatologists or radiologists.

OA Pathology on MRI
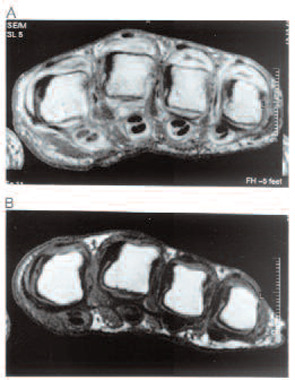
OA is a clinical syndrome for both patients and clinicians. MRI has been a major step forward in understanding the whole organ nature of the structural OA process. However—unlike RA, where MRI has helped simplify our understanding of pathogenesis and treatment response—in OA, we are just beginning to understand the complex interrelationship of pathological processes in multiple tissues. (See Figure 2, right.) MRI has demonstrated OA pathology in the following areas:7
Cartilage: This has long been the focus of much OA research. It has traditionally been evaluated in vivo by using conventional radiographs and measuring the tibio-femoral joint space as a surrogate measure. MRI allows us to examine the cartilage directly, showing that joint space narrowing involves meniscal degeneration and extrusion as well as cartilage loss.
Bone Marrow Edema: Bone marrow edema refers to a MRI appearance and not to a pan-arthritis, specific pathology. In OA, there is relatively little information on what areas of bone marrow edema refer to, and often they contain areas of bone cysts. From the limited information available, these may represent areas of necrosis and trabecular remodeling. They are more frequent in areas with increased Kellgren-Lawrence (KL) grade. MRI also shows bone attrition, and osteophytes are seen with much greater ease and frequency with MRI than with radiographs.
Meniscal Pathology: Large cohort studies employing MRI have demonstrated a vast amount of meniscal problems.
Soft Tissue Pathology: Synovitis is frequently seen using MRI. Ligament abnormalities, especially of the medial and lateral ligaments, are also commonly present and—surprisingly—abnormalities of the anterior cruciate ligament are quite common in large cohorts despite no history of significant knee injury. MRI can also demonstrate foreign bodies (although these are rarely of clinical significance).
MRI in OA Research
The wonderful sensitivity of MRI means we are able to phenotype OA better than before. We now need to understand the relative importance of the different pathological processes within the OA joint; this information is accruing from large clinical cohorts such as the NIH Osteoarthritis Initiative. Structure-pain studies will help us understand which features are most related to pain, allowing subsequent targeting of novel and existing therapies.
To date, the most work quantifying pathology has been on evaluating cartilage. Most cartilage measurement work employs image analysis with some element of manual alignment before automatic segmentation can occur. These systems now demonstrate good precision. In general, cartilage volume measurements are easier to obtain in flat areas such as the tibial plateau or central region of the femur, rather than in curved surfaces such as at the hip. Measurable cartilage parameters include total volume of cartilage, cartilage thickness, and cartilage signal intensity. The rate of cartilage loss is very important for studies that will examine the chondroprotective nature of drugs. Early studies suggest that the rate of cartilage loss is approximately 4% per year, but rates of loss may be lower than this in, for example, normally aligned knees.8 Higher rates may be obtained in studies by including subjects who are at risk of more rapid progression, such as those with higher KL grade or obesity. Some studies suggest that cartilage thickness may be a more important measure than cartilage volume over time.
It is unclear which tissue should be the focus for clinical trials. Symptom-modifying trials do not require MRI, and—for structure modifying trials—the plethora of MRI OA pathology will need to be validated against meaningful clinical endpoints. Until the most important feature or features seen on MRI are defined, most studies should evaluate multiple features.
It has been difficult to accurately quantify noncartilage features of the knee, although image analysis methods are being explored. However, the need to understand the whole organ pathology has driven development of a number of semiquantitative scores.8 All divide the knee into multiple anatomical compartments and measure multiple features on variable ordinal scales within each compartment. Further development will be required in the use of all these scales, including the best ways to aggregate scores across compartments.
MRI in OA Clinical Practice
At present, the role for MRI in OA clinical practice seems small. Osteoarthritis represents a syndrome of pain, functional loss, and reduced quality of life. Currently, the most important messages from MRI studies are the concepts we have learned. The whole organ nature was emphasized above, but MRI has also given us new clues on the sources of pain and a new understanding of the structural progression in OA. The most likely sources of pain appear to be the synovium and subchondral bone; both of these tissues are innervated, which adds validity to their importance. Bone marrow lesions and cartilage defects are associated with subsequent cartilage loss. The first real clinical use of MRI may be identifying patient subsets for targeted therapies, once these are available. Using MRI to determine meniscal pathology in the OA knee does not appear warranted. The major reason for doing so is if arthroscopy and debridement are required—a decision that should be made on clinical grounds of mechanical locking of the knee, not meniscal abnormality on MRI.
Conclusions
MRI is dramatically increasing our understanding of structural pathology in arthritis. In RA, we understand the links between inflammation and damage and can understand therapeutic response. MRI has provided excellent proof-of-concept tools that may move into clinical use. In OA, we are beginning to appreciate the extent of whole-organ pathology and have better tools to quantitate pathology, but more work is required to demonstrate relevant targets with clinically meaningful endpoints. Changes in MRI technology—especially in eMRI—may improve our day-to-day management of arthritis.
Dr. Conaghan is professor of musculoskeletal medicine at the University of Leeds (U.K.) and a consultant rheumatologist at Leeds Teaching Hospitals NHS Trust.
References
- Perry D, Stewart N, Benton N, et al. Detection of erosions in the rheumatoid hand; a comparative study of multidetector computerized tomography versus magnetic resonance scanning. J Rheumatol. 2005;32:256-267.
- Dohn UM, Ejbjerg BJ, Court-Payen M, et al. Are bone erosions detected by magnetic resonance imaging and ultrasonography true erosions? A comparison with computed tomography in rheumatoid arthritis metacarpophalangeal joints. Arthritis Res Ther. 2006;8:R110.
- Conaghan PG, O’Connor P, McGonagle D, et al. Elucidation of the relationship between synovitis and bone damage: a randomized magnetic resonance imaging study of individual joints in patients with early rheumatoid arthritis. Arthritis Rheum. 2003;48:64-71.
- Jimenez-Boj E, Nobauer-Huhmann I, Hanslik-Schnabel B, et al. Bone erosions and bone marrow edema as defined by magnetic resonance imaging reflect true bone marrow inflammation in rheumatoid arthritis. Arthritis Rheum. 2007;56:1118-1124.
- Ejbjerg BJ, Vestergaard A, Jacobsen S, Thomsen HS, Østergaard M. The smallest detectable difference and sensitivity to change of magnetic resonance imaging and radiographic scoring of structural joint damage in rheumatoid arthritis finger, wrist, and toe joints. Arthritis Rheum. 2005;52:2300-2306.
- Brown AK, Quinn MA, Karim Z, et al. Presence of significant synovitis in rheumatoid arthritis patients with disease-modifying antirheumatic drug-induced clinical remission. Arthritis Rheum. 2006;54:3761-3773.
- Conaghan PG. Is MRI useful in osteoarthritis? Best Pract Clin Rheumatol. 2006;20:57-68.
- Eckstein F, Mosher T, Hunter D. Imaging of knee osteoarthritis: data beyond the beauty. Curr Opin Rheumatol. 2007;19:435-443.
