Eosinophilia
LindseyRN / shutterstock.com
CHICAGO—High eosinophil counts that can’t be explained should concern rheumatologists and spark attempts to identify what’s happening, an expert said at the ACR State-of-the-Art Clinical Symposium in April.
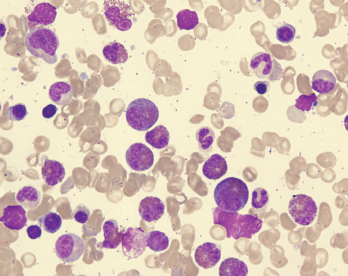
“Eosinophil counts over 1,500 (per microliter) should provoke worry,” said Bruce Bochner, MD, professor of medicine in allergy and immunology at Northwestern University Feinberg School of Medicine in Chicago. He cautioned that a patient with neutropenia will give a false increase in eosinophil percentage and, to obtain the true number, the white blood cell count should be multiplied by the eosinophil percentage.
The tip was among many offered in his talk for dealing with eosinophilia (counts of 500–1,500 per microliter) and hypereosinophilia (1,500 or more), which can be a manifestation of a variety of disorders, from allergies to drug reactions to leukemia.
The workup of a patient with eosinophilia or hypereosinophilia must be detailed and thorough, Dr. Bochner explained. The cause can be either primary or secondary, and can be characterized by its molecular cause or the organ involved. The treatment depends on the root cause, and expanding therapy options, he said.
“Whenever possible, go back and try to figure out when the eosinophilia or hypereosinophilia began,” he said. “There may be a new drug. There may be associated travel. There may be
something that is easily reversible that you’ll pinpoint.”
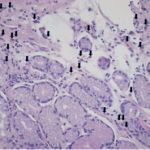
Hypereosinophila in a patient with gastrointestinal symptoms should prompt concern for eosinophilic gastritis, he said.
Two types of eosinophilia due to helminths that “you don’t want to miss” are Strongyloides stercoralis and Ascaris lumbricoides. Even though they are typically contracted in tropical climates, patients can be infected in regions of the U.S., so travel outside the country isn’t required. Strongyloides can disseminate and be lethal, especially if the patient is misdiagnosed and treated with corticosteroids, Dr. Bochner said.
Drug reactions with eosinophilia and systemic symptoms (DRESS) are typically marked by a measles-like rash starting two to eight weeks after taking the culprit drug and can prove life threatening, although the mechanisms at play are not well understood, he said.
‘In many of these conditions, one of the deadliest complications is endomyocardial involvement.’ —Dr. Bochner
In hypereosinophilia with myeloproliferative features, a gain-of-function deletion mutation has been identified, and the kinase inhibitor imatinib has yielded curative responses. This disorder tends to respond poorly to corticosteroids, Dr. Bochner said.
The lymphocytic variant, which can transform to malignancy, is mainly treated with corticosteroids, eventually combined with interferon alpha or other agents.
Dr. Bochner has co-authored a paper on when to consider specific tests in patients with hypereosinophilia syndrome (HES) and suggested it as a guide.1
“In many of these conditions, one of the deadliest complications is endomyocardial involvement—that’s why troponin is on this list of potential tests to order. Some of the worst patients I’ve seen had CBCs [complete blood counts] without a differential in the emergency [department], had chest pain, had normal coronary arteries by catheterization and turned out to have HES with cardiac involvement. The troponin was not due to ischemia, but instead was due to eosinophils infiltrating the myocardium,” he said.
In recent years, several anti-eosinophil therapies have been approved for the treatment of eosinophilic asthma, including mepolizumab, resluzumab and benralizumab. Others in development include dexpramipexole, an oral agent related to the existing drug pramipexole, a dopamine agonist that was inadvertently found to reduce eosinophil numbers and anti-Siglec 8, a monoclonal antibody that targets eosinophils and mast cells. Although none of these are approved by the U.S. Food & Drug Administration for HES treatment, published data suggest some agents have efficacy, Dr. Bochner said.
He said answers to some key questions could help improve treatment of hypereosinophilia-related disorders.
“I wish we had better biomarkers for assessing disease activity,” he said. “We all follow the eosinophil counts and that’s about as good as it gets. I wish we had less invasive ways of imaging eosinophilic inflammation instead of having to do biopsies. We still don’t understand what causes eosinophil activation in these disorders, or what perpetuates it.”
Note: Dr. Bochner is a consultant for GlaxoSmithKline, AstraZeneca and Teva Pharmaceutical Industries, which develop drugs for hypereosinophilia disorders, and he’s a co-holder of Siglec-8 patents, entitling him to a share of future royalties on products protected by those patents.
Thomas R. Collins is a freelance writer living in South Florida.
References
- Khoury P, Bochner BS. Consultation for elevated blood eosinophils: Clinical presentations, high value diagnostic tests, and treatment options. JACI-In Practice. 2018. In press.