MADRID—Nonsteroidal antiinflammatory drugs (NSAIDs) might still have a role in the treatment of axial spondylarthritis, an expert said here at the European League Against Rheumatism (EULAR) 2013 Annual European Congress of Rheumatology, held June 12–15. But other drugs are quickly being explored, with the understanding of the effectiveness of tumor necrosis factor (TNF) inhibitors, as well as other biologics, expanding all the time, others said.
Role of NSAIDs
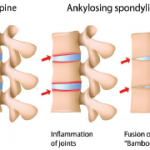
Nigil Haroon, MD, PhD, assistant professor of rheumatology at the University of Toronto, said the recent INFAST trial suggests that there might be a role for NSAIDs early in the treatment of patients with ankylosing spondylitis (AS).
Early AS patients—with an average disease duration less than two years, and who had not been on a maximal dose of an NSAID previously—were given either both naproxen and infliximab or naproxen and placebo. Their infusions were stopped at 24 weeks and response was assessed after 28 weeks.1
Researchers found that 62% of the patients were in partial remission in the naproxen–infliximab group, compared to about 35% of the naproxen–placebo group. Dr. Haroon noted that the remission rate in the naproxen–placebo group was relatively high.
“Maybe by diagnosing and treating these patients early, we may get significant benefit just from antiinflammatories alone,” Dr. Haroon said.
Dr. Haroon pointed to a 2005 study as most compelling on the disease-modifying potential of NSAIDs. Those on a continuous dose of NSAIDs showed significantly less radiographic progression than those taking NSAIDs as needed.2
Further analysis showed that the difference between the groups was limited to those with elevated C-reactive protein (CRP) at baseline. “If you have a predictor of progression (high CRP or syndesmophytes on X-ray) right at the beginning, then you’re more likely to respond with antiinflammatories, and progress less,” Dr. Haroon said. Researchers have also found that the lower the dose, the more likely patients are to progress.
There seems to be a biologic basis for this disease-modifying potential of NSAIDs. Bone density and osteoblastic activity have been shown to be impaired by systemic NSAID application in a mouse model.3 But, he said, the NSAID effect was not replicated in a large study led by Dr. Haroon, with participating centers from Canada and the U.S.
Another factor that can’t be ignored, he said, is cost, which is “a big advantage for naproxen.”
“That’s something you should always consider when you come up with guidelines and treatment recommendations,” he said.
In the end, when determining the role of NSAIDs, physicians have to consider several factors—the symptomatic state of the patient, the likelihood of radiographic progression, the risks of continuous NSAID treatment to the patient, and the treatment alternatives, Dr. Haroon said.
How Many TNF Inhibitors to Try?
Elisabeth Lie, MD, PhD, of the rheumatology department at Diakonhjemmet Hospital in Oslo, Norway, turned to TNF-inhibitors, discussing the potential benefits of switching from one to another.
Trying a second TNF inhibitor is an option many patients want to consider, since many of them won’t respond to the first—and Assessment of Spondyloarthritis International Society (ASAS)–EULAR recommendations from 2010 advise switching to a second TNF blocker, especially in patients who have failed on a first due to a loss of response.
Across eight studies on a variety of TNF inhibitors, the ASAS20 response rate was found to range from 60% to 70%, and the ASAS40 found to be 40% to 50%, Dr. Lie said. “This, then, means that there are at least 30% of patients not being counted as responders in these studies,” Dr. Lie said.
Antibodies to TNF inhibitors have been found to be a culprit in loss of response, she noted. Researchers found an ASAS20 response rate of 74% in patients with no antiinfliximab antibodies, but only a 9% rate in those with antibodies.4 A similar pattern was found in patients taking adalimumab.5
In RHAPSODY, a 12-week study of adalimumab in AS patients, included 1,250 patients—326 of whom had prior use of infliximab, etanercept, or both. One of the predictors of achieving a response was a patient being TNF naive.6
Another study—DANBIO—found lower response rates in those receiving a second TNF inhibitor—37% on Bath Measures on Ankylosing Spondylitis Disease Activity Index (BASDAI)—compared to those receiving their first—54%.
RHAPSODY’s data show that the reason for the switch can be a powerful predictor of the response on a second TNF inhibitor. The BASDAI50 response rate was 26% for those who switched because of a lack of response, compared to 43% for those who switched because of a loss of response and 39% for those who switch because they were intolerant. For ASAS20, those rates were 26% for lack of response, 42% for loss of response, and 46% for intolerance.
“Response rates,” Dr. Lie said, “were lower in those who had registered primary lack of response to the first TNF inhibitor as compared to those who had either loss of response or intolerance.”
New Therapies Under Investigation
Joachim Sieper, MD, professor of rheumatology at Charite University Hospital in Berlin, said that, beyond TNF inhibitors, there is not much that is proven in the way of biologics in axial spondolytis. But several prospects are on the horizon.
Abatacept, anti–IL-6R-antagonists, and anakinra, an IL-1-receptor antagonist, have been shown not to be effective.
Rituximab might be one avenue that deserves to be explored further, he said. A study—involving 10 patients who had never tried a TNF blocker and 10 with whom a TNF blocker had failed—showed promise among the TNF-naive patients. In that group, at Week 24, 50% had achieved an ASAS20 response, 40% an ASAS40 response, and 50% a BASDAI50 response.7
“I think the data would justify to go the next step, to do a small, placebo-controlled trial,” he said.
In his own lab, there are plans to further explore ustekinumab, an interleukin (IL) 23 blocker, after a trial of 20 patients with active AS showed benefit, Dr. Sieper said. The patients had shown an inadequate response to two more NSAIDs taken for at least two weeks or demonstrated an intolerance or contraindication to them.
In the pipeline, Dr. Sieper said, are several studies that are ongoing or are about to begin. They include trials on anti–IL-17 and anti–IL-23 drugs, as well as apremilast, a phosphodiesterase inhibitor, and tofacitinib, a JAK inhibitor.
There is a lot of activity, he said. But, he added, “TNF blockers are still the only proven biologic to be effective in AS if conventional treatment fails.”
Thomas Collins is a freelance medical writer based in Florida.
References
- Sieper J, Lenaerts J, Wollenhaupt J, et al. Efficacy and safety of infliximab plus naproxen versus naproxen alone in patients with early, active axial spondyloarthritis: Results from the double-blind, placebo-controlled INFAST study, Part 1. Ann Rheum Dis. 2013 May 21. [Epub ahead of print]
- Wanders A, Heijde Dv, Landewé R, et al. Nonsteroidal antiinflammatory drugs reduce radiographic progression in patients with ankylosing spondylitis: A randomized clinical trial. Arthritis Rheum. 2005;52:1756-1765
- Spiro AS, Beil FT, Baranowsky A, et al. BMP-7-induced ectopic bone formation and fracture healing is impaired by systemic NSAID application in C57BL/6-mice. J Orthop Res. 2010;28:785-791.
- de Vries MK, Wolbink GJ, Stapel SO, et al. Decreased clinical response to infliximab in ankylosing spondylitis is correlated with anti-infliximab formation. Ann Rheum Dis. 2007;66:1252-1254.
- de Vries MK, Brouwer E, van der Horst-Bruinsma IE, et al. Decreased clinical response to adalimumab in ankylosing spondylitis is associated with antibody formation. Ann Rheum Dis. 2009; 68:1787-1788
- Rudwaleit M, Claudepierre P, Wordsworth P, et al. Effectiveness, safety, and predictors of good clinical response in 1250 patients treated with adalimumab for active ankylosing spondylitis. J Rheumatol. 2009;36:801-808.
- Song IH, Heldmann F, Rudwaleit M, et al. Different response to rituximab in tumor necrosis factor blocker-naive patients with active ankylosing spondylitis and in patients in whom tumor necrosis factor blockers have failed: A twenty-four-week clinical trial. Arthritis Rheum. 2010;62:1290-1297.