MADRID—New imaging technologies in spondylarthritis (SpA)—from diffusion-weighted imaging to ultrasonography—are being studied and refined, but much is yet be understood, said Anne Grethe Jurik, MD, clinical associate professor of diagnostic radiology at Aarhus University in Denmark, here at the European League Against Rheumatism (EULAR) 2013 Annual European Congress of Rheumatology, held June 12–15.
Imaging in SpA
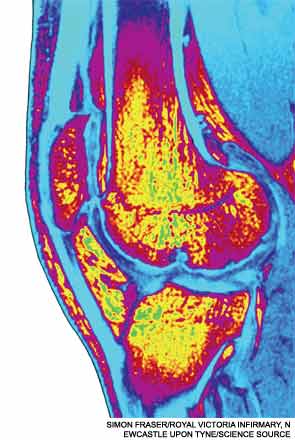
The mainstay, magnetic resonance imaging (MRI), is a sensitive technique, but normal variants can sometimes lead radiologists and physicians astray, resulting in false positives, she cautioned.
Dr. Jurik’s review came as part of a session on imaging techniques on SpA, osteoarthritis, and gout.
MRI activity changes in the sacroiliac joints (SIJs) that are consistent with SpA can also occurin individuals without SpA. Single lesions on MRI suggestive of inflammation have been reported in the SIJs in up to a quarter of young patients with mechanical back pain and healthy controls, studies have found.1
Normal variants can occur fairly frequently. Accessory sacroiliac joint has been seen in as many as 19% of subjects, iliosacral complex in 10%, and bipartite iliac bony plate in nearly 6%, Dr. Jurik said.
The Assessment of Spondyloarthritis International Society (ASAS) criteria for sacroiliitis is bone marrow edema seen using short inversion time recovery (STIR) or osteitis on T1 postcontrast images located in typical subchondral or periarticular bone areas—but the criteria don’t include structural changes, even though those can occur within the first two years of the disease.
“There is a need for revision of the ASAS MR criteria, with inclusion of structural changes,” Dr. Jurik said.
As for other techniques, whole-body MRI (WB-MRI) of the sacroiliac joints and spine can reliably detect inflammatory SIJs and spinal lesions in SpA patients, compared with conventional MRI, she said. There also might be value in imaging the anterior chest wall and enthesitis with this method, she said.
Studies have found that WB-MRI, including postcontrast sequence, detects significantly more areas of synovitis and enthesitis in SpA than through clinical means, except in the hands and feet, she said.2
Dr. Jurik said diffusion-weighted MRI, based on the movement of water protons, might be a way to diagnose early active sacroiliitis and includes the possibility of objectively quantifying inflammation using apparent diffusion coefficient values.

