MADRID—Progress continues to be made in efforts to improve management of osteoarthritis and generate new therapies, researchers reported here at the European League Against Rheumatism (EULAR) 2013 Annual European Congress of Rheumatology, held June 12–15, with continued evidence on the benefits of knee distraction and progress in harnessing the effects of stem cells.
Distraction Frame Can Encourage Joint Repair
Simon Mastbergen, PhD, assistant professor of rheumatology at the University Medical Center Utrecht in The Netherlands, reviewed the apparent benefits of knee joint distraction in late-stage osteoarthritis.
In the procedure, pins are drilled through the bone just above and below the knee, and a spring-loaded “distraction frame” is fitted onto the leg, taking a load off the knee by creating a small space between its cartilaginous surfaces. The frame stays on for two months.
The technique has proven to have long-term clinical effectiveness for end-stage ankle osteoarthritis.
His research group has found improvements in the thickness and volume of knee cartilage after a year and the benefit has been sustained through five years, although results beyond five years remain unclear.
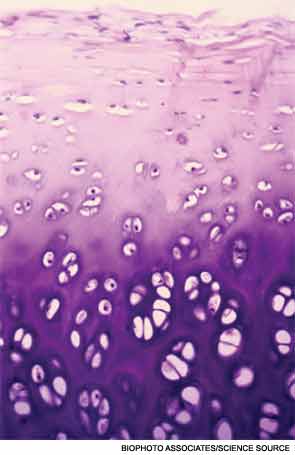
X-rays taken while patients were bearing full weight on the knee showed that the tissue that had formed worked structurally.1 Plus, Dr. Mastbergen said, collagen-type II biomarkers increased during this healing process, suggesting that the newly formed cartilage tissue is hyaline cartilage, and not more spongy fibrocartilage.
Several factors are likely at work in this healing process, Dr. Mastbergen said. The absence of stress on the joint encourages healing, he said. Plus, intermittent, intraarticular fluid pressure occurs because patients are encouraged to walk while in the frame. “This is important, first of all, for the nutrition of cartilage, but also, it appears from the in vitro [analyses] that there is an effect in the cartilage itself,” he said.
There is also temporary periarticular osteopenia in which “sclerotic bone becomes less sclerotic,” he said. “The bone gets a little bit softer and there’s a little bit of softening in the mechanical stress on the cartilage itself.”
Researchers have also found that mesenchymal stem cells adhere to a far greater degree to a diseased distracted joint than a nondistracted one.
Further study on the mechanics of the process—from the absence of stress to the trophic factors at work—can help refine treatment approaches, he said. “Now we have a system where we at least see the regeneration of the joint,” Dr. Mastbergen said.
Dr. Mastbergen was asked why he thinks the procedure hasn’t been adopted more widely, since it really does appear that regeneration is taking place.
“People need to be convinced whether it’s actually happening—for such a long time there was a belief that it couldn’t be regenerated,” he said. “I think the last couple of years … there is more belief in the treatment and we’re now working together with some of our collaborators [in the U.S.] and other groups [in Japan and Germany] to actually get it more implemented.”
He added, “We try to talk about it as much as possible.”
Mesenchymal Stem Cells to Drive Repair
Elena Jones, PhD, associate professor at the Leeds Musculoskeletal Biomedical Research Unit in Leeds, U.K., discussed the potential of a “one-step” surgical procedure using mesenchymal stem cells (MSCs)—known to drive bone and cartilage repair—in patients with osteoarthritis.
The procedure is based on findings that MSCs exist in abundance in bone, the synovium, and synovial fluid, so that “the use of exogenously added, culture-expanded cells might not be necessary,” she said.
“We believe, in our lab, that instead of going this long way around in tissue-culture expansion, we could simply modulate MSC attachment to cartilage defects. Alternatively, we could extract MSCs from fresh tissue, and then replant in a one-day procedure, bypassing all long culture-expansion stages, making therapy much more cost effective—and also a single-surgery procedure, which is very beneficial,” Dr. Jones said.
She and her research team have developed a flow cytometry assay, “in which, in 40 minutes, we can tell the dose of MSCs in this particular sample of bone marrow aspirate,” she said. There has been excellent correlation between their assay and the typical, two-week-long colony assay to count MSCs.
“So, we actually think that tissues currently discarded by surgeons can be used in the future for repairing bone and cartilage,” she said, adding that allogeneic applications might be possible as well.
Does Synovium Hold the Key to Cartilage Repair?
Cosimo De Bari, MD, PhD, Professor and Chair of Medicine and Therapeutics at the University of Aberdeen, talked about the importance of the synovium as a producer of mesenchymal stem cells for cartilage repair—calling them possibly the “ideal chondroprogenitor” in this process.
Part of what makes the synovium so powerful in this regard, he said, is that it shares a common embryonic derivation with the joint surface.
Dr. De Bari and his research team published findings in 2011 showing the presence of endogenous resident MSCs in adult mouse knee joints—slow-cycling cells that proliferate and differentiate after injury to the joint.2
“The questions that we’re trying to address [are], What is the role of MSCs on joint homeostasis?” he said. “What is their physiological role? What is the role of MSCs on the pathogenesis of osteoarthritis and rheumatoid arthritis?”
Further understanding of the role of MSCs could be the foundation for the future of disease-modifying drugs in rheumatic diseases, Dr. De Bari said.
Thomas Collins is a freelance medical writer based in Florida.
References
- Intema F, Van Roermund PM, Marijnissen AC, et al. Tissue structure modification in knee osteoarthritis by use of joint distraction: An open 1-year pilot study. Ann Rheum Dis. 2011;70:1441-1446.
- Kurth TB, Dell’accio F, Crouch V, Augello A, Sharpe PT, De Bari C. Functional mesenchymal stem cell niches in adult mouse knee joint synovium in vivo. Arthritis Rheum. 2011;63:1289-1300.
