MADRID—Assessing whether patients with rheumatic diseases have peripheral neuropathy—and determining the right treatment course—can a somewhat complicated process, but it can be a key part of a patient’s overall care, experts said here at the European League Against Rheumatism (EULAR) 2013 Annual European Congress of Rheumatology, held June 12–15.
Peripheral neuropathy is common in patients with a rheumatic disease, and addressing these concerns involves answering several questions, said Yvonne Lee, MD, assistant professor of medicine at Harvard Medical School in Boston.
First, does the patient actually have a peripheral neuropathy? Which tests should be done to determine this? How should they be interpreted? Finally, if the patient does have a peripheral neuropathy, is it because of the rheumatic disease, medications, or is it just coincidental?
Diagnosis
The diagnostic approach involves discerning a nervous system abnormality from conditions with similar symptoms (e.g., myopathies) and distinguishing a peripheral neuropathy from a central nervous system disease.
Neuropathy can be categorized as mononeuropathy or mononeuritis multiplex (focal or multifocal involvement of one or more nerve trunks, due mostly to entrapment or vasculitis, and with acute or subacute onset); polyneuropathy (symmetrically distributed, often distally distributed, and with gradual onset); or polyradiculoneuropathy (diffuse involvement and usually inflammatory in origin).
Initial diagnostic methods usually involve laboratory testing, including a complete blood count, creatinine, liver enzymes, fasting glucose level, and erythrocyte sedimentation rate.
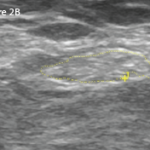
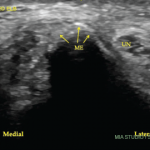
Physicians can then turn to electrodiagnostic studies to confirm a diagnosis of peripheral neuropathy, assess the extent of it, determine whether it is axonal or demyelinating, and assess its severity, Dr. Lee said.
Nerve biopsy, she said, can help in diagnosing an inflammatory neuropathy, especially to demonstrate vasculitis, but shouldn’t be done before adequate clinical, laboratory, and electrophysiologic studies have been done.1 Results are often nonspecific, and complications, such as sensory loss and/or unpleasant abnormal sensations, are common.2
Common types of neuropathy seen in patients with rheumatic diseases include entrapment neuropathy, such as carpal tunnel and ulnar nerve entrapment; inflammatory neuropathies, such as Sjögren’s syndrome, systemic vasculitides, and systemic lupus erythematosus (SLE); and small-fiber neuropathy. Although originally linked mainly with diabetes, small-fiber neuropathy has also been reported in association with SLE, rheumatoid arthritis, sarcoidosis, and celiac disease.
Medication-induced neuropathies also should also be included in the differential diagnosis, Dr. Lee said. Patients at risk for a leflunomide-induced neuropathy include the elderly, diabetics, those on neurotoxic drugs, and those with risk factors such as alcoholism and renal impairment.
She also noted that 23 cases of Guillian-Barré Syndrome, linked to tumor necrosis factor (TNF) antagonists have been reported in the literature, though it is unclear whether the link is with the drug, the disease, or with associated infections.3
“Consider medications, such as leflunomide and TNF antagonists,” Dr. Lee said, “as potential causes of peripheral neuropathy.”
Treatment Options
Franz Blaes, MD, of the department of neurology at Gummersbach Hospital in Germany, said the treatment approach to peripheral neuropathy in patients with rheumatic diseases is not a simple thing.
“The problem is, if you’re going to treat peripheral neuropathy in rheumatic disease, we need a type of clear classification,” he said. “And the question is: Do we have one? Maybe not, maybe we have one. I’m not sure about it.”
Patients can be classified neither as a rheumatic disease patient, nor as a patient with a neurological syndrome, but as both, he said.
Patients with inflammatory rheumatic disease—those with Sjögren’s syndrome, scleroderma, or lupus, for instance—who have a demyelinating neuropathy often respond well to steroids or intravenous immunoglobulin (IVIg), he said.
Those with pure autonomic neuropathy—rare in inflammatory rheumatic disease patients—might respond to steroids, IVIg, or plasmapheresis.
For nonsystemic vasculitic neuropathy, steroids alone are the first-line therapy, but a combination of steroids and cyclophosphamide (CYC) or methotrexate can be used in cases with rapid progression. IVIg, plasmapheresis, or rituximab can be tried in refractory cases, Dr. Blaes said.
In cases of mixed cryoglobulinemic vasculitis with neuropathy, interferon-alpha has been shown to have little effect on neuropathy. For a steroids–CYC combination, there are no randomized controlled trials or case series available to prove their effects. Plasma exchange, Dr. Blaes said, has been effective in some patients. In one trial, 60% of patients improved on rituximab.4
In another study, 19 out of 22 patients with systemic vasculitic peripheral neuropathy—in seven published case series—improved after taking rituximab.5
For those with small-fiber neuropathy, steroids plus neuropathic pain treatment can be effective, Dr. Blaes said.
“The treatment of neuropathies in rheumatology cannot be based only on the underlying vasculitic disease or the underyling neurological syndrome,” he said. “You have to take into account both sides.”
Thomas Collins is a freelance medical writer based in Florida.
References
- Mellgren SI, Lindal S. Nerve biopsy—some comments on procedures and indications. Acta Neurol Scand Suppl. 2011;191:64-70.
- Ruth A, Schulmeyer FJ, Roesch M, Woertgen C, Brawanski A. Diagnostic and therapeutic value due to suspected diagnosis, long-term complications, and indication for sural nerve biopsy. Clin Neurol Neurosurg. 2005;107:214-217.
- Alvarez-Lario B, Prieto-Tejedo R, Colazo-Burlato M, Macarrón-Vicente J. Severe Guillain-Barré syndrome in a patient receiving anti-TNF therapy. Consequence or coincidence. A case-based review. Clinc Rheumatol. 2013 May 11. [Epub ahead of print]
- Ferri C, Cacoub P, Mazzaro C, et al. Treatment with rituximab in patients with mixed cryoglobulinemia syndrome: Results of multicenter cohort study and review of the literature. Autoimmun Rev. 2011;11:48-55.
- Eriksson P. Nine patients with anti-neutrophil cytoplasmic antibody-positive vasculitis successfully treated with rituximab. J Intern Med. 2005;257:540-548.