James Cavallini / Science Source
Baltimore—Rheumatologists and meteorologists share more in common than you might suspect, said Dr. Rebecca Manno, assistant professor of medicine for the Division of Rheumatology at Johns Hopkins University, Baltimore, and assistant director of the Johns Hopkins Vasculitis Center. At a March 8 meeting of the Maryland Society for the Rheumatic Diseases, Dr. Manno used the weather as an analogy for understanding updates on classification, diagnosis and treatment of giant cell arteritis (GCA) and topics to watch for in the coming year.
“This is an exciting and unprecedented time for GCA,” Dr. Manno said. “There have been incredible advances in the diagnosis and treatment of this potentially devastating disease, and these are directly affecting the lives of patients in a positive way.”
Classification & Diagnosis
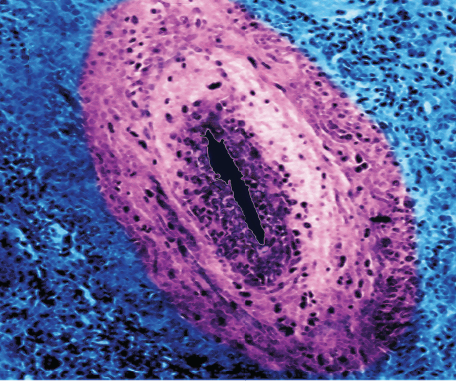
Just as the categorization and naming of hurricanes is important in correctly identifying these phenomena, said Dr. Manno, so too is vasculitis nomenclature. The Revised International Chapel Hill Consensus Conference of 2012 identified GCA as one of two large-vessel vasculitides (the other being Takayasu’s arteritis), yet Dr. Manno pointed out that a large-vessel vasculitis, such as GCA, can also affect medium and small arteries. The term temporal arteritis, which is often used interchangeably with GCA, can be misleading both because other vasculitides, such as polyarteritis nodosa, can affect the temporal arteries and because exclusive large-vessel involvement may be seen in GCA even when temporal artery involvement is scant or absent.
Classification criteria for GCA are outdated, and diagnostic criteria do not exist. To address this important unmet need, the multinational, observational Diagnostic and Classification Criteria in Vasculitis Study (DCVAS) has developed updated diagnostic and classification criteria for large-vessel vasculitis, using new techniques and incorporating advances in imaging. These provisional criteria and data will be presented at the 2018 ACR/ARHP Annual Meeting in October.
Dr. Manno noted that, similar to how meteorological imaging used to characterize weather events has greatly advanced in recent years, magnetic resonance imaging (MRI) and positron emission tomography/computed tomography (PET/CT) represent a new frontier in GCA diagnostics. Conventional and CT angiography can assist in the diagnosis of large-vessel GCA, but MRI/ magnetic resonance angiography (MRA) is a non-invasive procedure that does not expose patients to radiation and can identify manifestations, such as aortitis or subclavian stenosis, that may have important implications for the patient. MRI/MRA may be of particular utility when the clinical history is consistent with GCA but the temporal artery biopsy is negative, although Dr. Manno cautioned that artifacts in MRA with contrast, such as subclavian pseudostenosis (which is a mimic of stenosis due to focal irregularity of the subclavian artery from residual contrast remaining in the adjacent vein), can confound the picture. PET/CT is another technique that can identify large-vessel vasculitis by demonstrating FDG avidity in blood vessels, thereby potentially indicating active disease.

