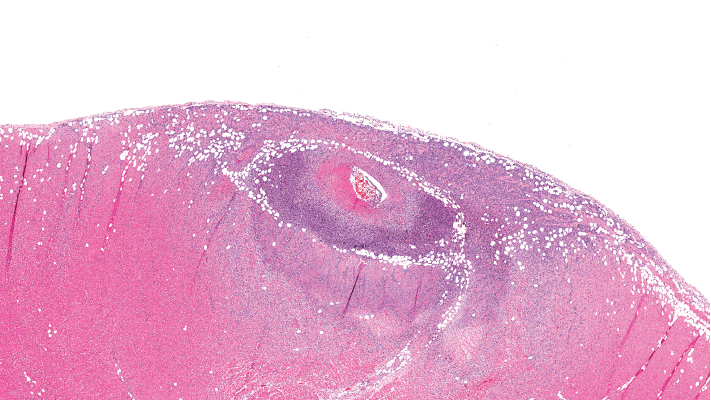
This image depicts severe arteritis of the coronary artery with inflammation and thrombosis, with extension into the myocardium.
A proposed model to predict the risk of giant cell arteritis (GCA) prior to a temporal artery biopsy could help triage patients and guide decision making about the need for biopsy or monitoring (see Figure 1).
There’s no specific biomarker for GCA, and GCA can be a “diagnostic conundrum, especially when it presents in an occult or atypical fashion,” according to the researchers who published the development and validation data on their multivariable prediction model in a recent issue of Clinical Ophthalmology.1
Edsel Ing, MD, MPH, an ophthalmologist at Michael Garron Hospital and associate professor at the University of Toronto, and his colleagues note that even though several clinical prediction rules in the diagnosis and management of patients with suspected GCA exist, few were developed using more than 500 temporal artery biopsies or 100 biopsy-positive GCA cases, and few included external validation. The group’s research was compliant with the TRIPOD Initiative, a set of recommendations for reporting research that develops, validates or updates a prediction model so that bias risk and potential usefulness of the model can be adequately assessed.
The dearth of validated, TRIPOD-compliant prediction models for GCA that predict the risk prior to temporal artery biopsy prompted the research, Dr. Ing says. “GCA can be very difficult to diagnose without a biopsy. Sometimes, we look at blood tests, but how significant are the serology results compared with the patient’s symptoms? If a 60-year-old patient has a new-onset headache but blood tests are normal, compared to a 65-year-old patient with abnormal serology but no headache, determining the relative risk for GCA is problematic.”
Objective vs. Subjective Variables
Dr. Ing’s research analyzed the predictive value of objective and subjective variables that could potentially predict which patients are at higher risk of having biopsy-proven GCA. The investigators performed a retrospective review of case records of consecutive adult patients undergoing temporal artery biopsy for suspected GCA at seven secondary/tertiary care referral clinics. The researchers retrieved records from four medical centers in Canada, the U.S. and Switzerland. Forty-eight percent of the patients had been referred by ophthalmologists, and the rest by rheumatologists, internal medicine physicians or primary care centers.
All patients undergoing temporary artery biopsy for suspected GCA within two weeks of steroid initiation were eligible for the study. The pathologic diagnosis was considered the final diagnosis. Healed arteritis was considered positive for GCA in the research, and any case with an indeterminate pathologic diagnosis was considered negative for GCA. A review of 688 patients undergoing temporal artery biopsy yielded 530 cases with complete data. From the cohort of 530 cases, negative temporal artery biopsy results were reported for 397 patients and positive biopsies for 133 patients. The researchers performed multiple imputation for the missing data.

