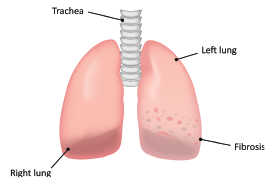
Interstitial lung disease (ILD) is a heterogeneous group of lung parenchymal disorders that share several clinical, radiologic and histopathologic features, and are therefore grouped together.1 ILD can occur in association with most rheumatic connective tissue diseases (CTDs), but patients with systemic sclerosis, polymyositis, dermatomyositis and rheumatoid arthritis have the highest risk of developing ILD.2
A multidisciplinary panel in 2017 reported that around 10% of patients with rheumatoid arthritis (RA) have clinical ILD. Another 30% may have subclinical ILD, indicating that about 40% of RA patients may have some form of lung involvement during the course of their disease.2
Patients may present with ILD concurrently with their RA diagnosis, develop ILD along the course of RA or, less frequently, present first with ILD without typical RA symptoms at the time of diagnosis.1,3 The fact that several disease modifying anti-rheumatic drugs (DMARDs) have been implicated as a cause of ILD adds to the conundrum.4
This poses a significant challenge when choosing the most appropriate DMARD for patients with RA.
Methotrexate
joshya / shutterstock.com
Methotrexate is the usual first-line treatment and the cornerstone of therapy for RA.5 It has been widely reported as a cause of ILD and acute interstitial hypersensitivity pneumonitis.6-8 Lung toxicity due to methotrexate can occur at any time during the course of treatment, which makes it difficult to assess its precise incidence.4,9
More recent data indicate the risk of ILD with methotrexate is not as high as previously thought.10 In fact, methotrexate may not increase the frequency of ILD at all. The propensity of RA to cause ILD may be responsible for the earlier overestimates.10
On the other hand, several reports have indicated the presence of pre-existing ILD (clinical or sub-clinical) is a risk factor for hypersensitivity pneumonitis.11-13
When ILD is not present before instituting methotrexate treatment, it is often challenging to distinguish methotrexate-induced lung toxicity from RA-associated ILD. Even though some of the reluctance to use methotrexate may be misplaced, situations with pre-existing ILD may require consideration of alternatives to methotrexate.
Leflunomide
Leflunomide is an inhibitor of pyrimidine synthesis, which is thought to be the mechanism for its anti-inflammatory and immunomodulatory properties. It is available in doses of 10 mg and 20 mg, taken as a daily tablet.
Leflunomide was first introduced in the 1990s and initial reports indicated a very low incidence of ILD.4
The initial concerns regarding lung toxicity with leflunomide were raised on the basis of cases reported in Japan, followed by cases from Korea and other parts of the world.14-18
The authors of a systematic review in 2014 concluded that leflunomide can be associated with ILD in RA and that it can be potentially fatal and may present more acutely than methotrexate-induced pneumonitis.4
However, they do acknowledge the difficulty of distinguishing lung toxicity from leflunomide from RA-ILD. Additionally, since the majority of patients who developed lung toxicity on leflunomide in various studies have either been exposed to methotrexate in the past or had pre-existing ILD, or both, it is difficult to conclusively implicate leflunomide as a cause of lung toxicity.
Raj et al. concluded in a systematic review in 2013 that leflunomide can cause ILD and that most patients develop lung toxicity within three months of starting it.19 They note that patients with pre-existing ILD are most likely to develop lung toxicity.
In 2006, a case control study by Suissa et al. found 74 cases of serious ILD out of a total of 62,734 patients with RA who were prescribed DMARDs.18 The risk of ILD increased with the use of leflunomide.
Interestingly, in patients who had no previous exposure to methotrexate and no history of ILD, the risk associated with leflunomide was not elevated. Additionally, patients who had a prior history of ILD were twice as likely to be prescribed leflunomide than any other DMARD. Therefore, the authors conclude the reports of ILD associated with leflunomide use are likely due to channeling patients with ILD or a history of methotrexate use to treatment with leflunomide.
A meta-analysis of double-blind, randomized controlled trials of leflunomide vs. placebo or active comparator drugs by Conway et al. in 2016 evaluated a total of eight studies that met the inclusion criteria, and four of these had placebo comparators. Studies with fewer than 50 subjects or duration less than 12 weeks were excluded.20
The results show no increase in total adverse respiratory events with leflunomide relative to comparator drugs. In fact, leflunomide is associated with a decreased risk of non-infectious adverse events. The authors acknowledge that in most of the individual, randomized controlled trials included, the number of patients was relatively small, thus reducing the ability to detect small increases in risk that may be clinically significant. However, the data from these trials were pooled in the meta-analysis, leading to increased power and equal distribution of bias. Although ILD can occur at any point along the course of RA and its treatment, the inclusion of randomized controlled trials at least 12 weeks or longer does counter some of the concerns raised specifically regarding leflunomide and lung toxicity.
Because RA is a systemic disease, it logically follows that control of overall disease activity should lead to a reduced risk of pulmonary involvement as well.
In Sum
Leflunomide is rarely the first DMARD used for treatment of RA and is, in fact, most often used after methotrexate has been discontinued for various reasons, or less often in combination with methotrexate, if methotrexate monotherapy is not adequate to control disease activity. Therefore, it may never be possible to determine the exact incidence of lung toxicity directly caused by leflunomide.
However, the newer data should help alleviate concerns of rheumatologists considering leflunomide as a viable conventional DMARD alternative to methotrexate in patients with ILD, before moving on to other more expensive biologic drugs.
Rajandeep Paik, MD, FACR, is a rheumatologist practicing in Malden, Mass. He works for Cambridge Health Alliance and is a lecturer in medicine at Harvard Medical School, Boston. Dr. Paik is board certified in rheumatology and internal medicine, and an ACR fellow.
References
- Fischer A, du Bois R. Interstitial lung disease in connective tissue disorders. Lancet. 2012 Aug 18;380(9842):689–698.
- Fischer A, Strek ME, Cottin V, et al. Proceedings of the American College of Rheumatology/Association of Physicians of Great Britain and Ireland Connective Tissue Disease-Associated Interstitial Lung Disease Summit: A multidisciplinary approach to address challenges and opportunities. Arthritis Rheumatol. 2019 Feb;71(2):182–195.
- Castelino FV, Varga J. Interstitial lung disease in connective tissue diseases: Evolving concepts of pathogenesis and management. Arthritis Res Ther. 2010;12(4):213.
- Roubille C, Haraoui B. Interstitial lung diseases induced or exacerbated by DMARDs and biologic agents in rheumatoid arthritis: A systematic literature review. Semin Arthritis Rheum. 2014 Apr;43(5):613–626.
- Singh JA, Saag KG, Bridges SL, et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Care Res (Hoboken). 2016 Jan;68(1):1–25.
- Lateef O, Shakoor N, Balk RA. Methotrexate pulmonary toxicity. Expert Opin Drug Saf. 2005 Jul;4(4):723–730.
- Cannon GW, Ward JR, Clegg DO, et al. Acute lung disease associated with low-dose pulse methotrexate therapy in patients with rheumatoid arthritis. Arthritis Rheum. 1983 Oct;26(10):1269–1274.
- Searles G, McKendry RJ. Methotrexate pneumonitis in rheumatoid arthritis: Potential risk factors. Four case reports and a review of the literature. J Rheumatol. 1987 Dec;14(6):1164–1171.
- Imokawa S, Colby TV, Leslie KO, Helmers RA. Methotrexate pneumonitis: Review of the literature and histopathological findings in nine patients. Eur Respir J. 2000 Feb;15(2):373–381.
- Fragoulis GE, Conway R, Nikiphorou E. 2019. Methotrexate and interstitial lung disease: Controversies and questions. A rarrative review of the literature. Rheumatology (Oxford). 2019 Nov 1;58(11):1900–1906.
- Ibfelt HE, Kart Jacobsen R, Kopp TI, et al. Treatment with methotrexate and risk of lung disease in patients with rheumatoid arthritis: A nationwide population-based cohort study from Denmark (abstract OP0232). Ann Rheum Dis. 2020;79(suppl 1):147–148.
- Saravanan V, Kelly CA. Reducing the risk of methotrexate pneumonitis in rheumatoid arthritis. Rheumatology (Oxford). 2004 Feb;43(2):143–147.
- Alarcón GS, Kremer JM, Weinblatt ME, et al. Risk factors for methotrexate-induced lung injury in patients with rheumatoid arthritis: A multicenter, case-control study. Ann Intern Med. 1997 Sep 1;127(5):356–364.
- Ochi S, Harigai M, Mizoguchi F, et al. Leflunomide-related acute interstitial pneumonia in two patients with rheumatoid arthritis: Autopsy findings with a mosaic pattern of acute and organizing diffuse alveolar damage. Mod Rheumatol. 2006;16(5):316–320.
- Wong SPY, Chu CM, Kan CH, et al. Successful treatment of leflunomide-induced acute pneumonitis with cholestyramine wash-out therapy. J Clin Rheumatol. 2009 Dec;15(8):389–392.
- Ju JH, Kim S-I, Lee J-H, et al. Risk of interstitial lung disease associated with leflunomide treatment in Korean patients with rheumatoid arthritis. Arthritis Rheum. 2007 Jun;56(6):2094–2096.
- Savage RL, Highton J, Boyd IW, Chapman P. Pneumonitis associated with leflunomide: A profile of New Zealand and Australian reports. Intern Med J. 2006 Mar;36(3):162–169.
- Suissa S, Hudson M, Ernst P. Leflunomide use and the risk of interstitial lung disease in rheumatoid arthritis. Arthritis Rheum. 2006 May;54(5):1435–1439.
- Raj R, Nugent K. Leflunomide-induced interstitial lung disease (a systematic review). Sarcoidosis Vasc Diffuse Lung Dis. 2013 Nov 22;30(3):167–176.
- Conway R, Low C, Coughlan RJ, et al. Leflunomide use and risk of lung disease in rheumatoid arthritis: A systematic literature review and metaanalysis of randomized controlled trials. J Rheumatol. 2016 May;43(5):855–860.

