NETs
The article reviews research findings on neutrophil dysregulation and NETs in SLE; the formation of NETs, including the unique form of cell death, NETosis; LDGs and vascular damage in SLE; NETs and autoantigen exposure; impaired NET clearance; and the link between NETs and inflammation and organ damage.
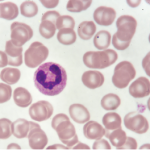
NETs are web-like structures comprising DNA, RNA, histones and anti-microbial proteins, “which are released to the extracellular space by activated neutrophils in response to a variety of microbial and sterile inflammatory stimuli,” Dr. Kaplan explains.
In SLE, the dysregulated formation and impaired clearance of NETs lead to their “accumulation within tissues and to their extended half-life in circulation, potentially contributing to perpetuating autoantigen generation and modification, inflammation and tissue damage,” Dr. Kaplan writes. “NETs may contribute to the pathogenesis of lupus nephritis, lupus-associated skin disease, thrombosis, vascular damage and tissue injury in various organs, including pregnancy complications, such as preeclampsia.”
When exposed to modified autoantigens, NETs may trigger the production of autoantibodies, including anti-double-stranded DNA and anti-nucleosome antibodies, “perpetuating the autoimmune responses in SLE,” Dr. Kaplan continues. NETs promote plasmacytoid dendritic cell activation in vitro and type I interferon (IFN) production, “driving systemic inflammation and amplifying immune dysregulation” in SLE.
NET Biomarkers
Elevated NET levels and LDGs have been linked to increased disease activity in patients with SLE. Measuring markers for NETs and LDGs may help diagnose and monitor disease activity, delivering insights into disease progression and treatment response.
Markers that identify NETs—detected in blood and tissue samples via several methods—include citrullinated histone-DNA complexes, DNA-MPO or DNA-neutrophil and elastase complexes. However, the use of cell-free DNA should be avoided as a sole marker because it is not a specific indicator of NET formation.
“Once properly validated, monitoring NET levels could provide valuable information for assessing disease progression and treatment response, “Dr. Kaplan writes. “NETs could be used to identify patients at risk of relapse and guide preemptive therapeutic interventions. Further, anti-NET antibodies targeting NET components, such as citrullinated histones and MPO, have emerged as potential biomarkers for lupus diagnosis and stratification,” and “studies have linked levels of LDGs to vascular damage.”
In the case study, the patient’s active disease was associated with the presence of elevated NETS and LDGs. “It is possible that these NETs have contributed to her active skin and joint disease, although tissue biopsies would have been needed to document their involvement,” Dr. Kaplan explains.