Jeffrey Siegel, MD, Assumes New Position as Director for New Office of Drug Evaluation Sciences at the FDA
 On Feb. 16, Jeffrey Siegel, MD, became the director of the recently created Office of Drug Evaluation Sciences at the U.S. Food & Drug Administration (FDA). The move, he says, “puts together many of the different things I’ve been most passionate about over the course of my career: applying science to drug development through biomarkers and other means; developing new outcome measures for clinical development programs in areas of unmet medical need, particularly rare diseases; and innovating clinical trial design.”
On Feb. 16, Jeffrey Siegel, MD, became the director of the recently created Office of Drug Evaluation Sciences at the U.S. Food & Drug Administration (FDA). The move, he says, “puts together many of the different things I’ve been most passionate about over the course of my career: applying science to drug development through biomarkers and other means; developing new outcome measures for clinical development programs in areas of unmet medical need, particularly rare diseases; and innovating clinical trial design.”
The position represents a return to the FDA after his time in industry. In 2010, Dr. Siegel left his position as clinical team leader at the FDA’s Center for Drug Evaluation and Research (CDER), Office of Drug Evaluation II, and Division of Anesthesia, Analgesia, and Rheumatology Products. He became the global lead for rheumatology and rare diseases for Genentech/Roche, where he was responsible for phase 3 clinical trials for new products and new indications for previously approved Genentech/Roche products. He then moved to Gilead, where he led translational medicine in the clinical research for inflammation group.
Now that he’s returned to the FDA, he is often asked why he spent time in industry; and conversely, why he has now returned to the FDA. “I had a great experience in industry,” Dr. Siegel says. He notes that although there are similarities between how industry and the FDA approach drug development, understanding that there are considerations and motivations unique to industry is important. He hopes to bring this understanding to the FDA, where certain policies are particularly helpful to incentivize companies to develop products for unmet medical needs.
Throughout his career, Dr. Siegel has found that focusing on what unifies different groups is an effective way to move forward. That unifying approach, he believes, can facilitate development of new, effective and safe treatments for patients.
Dr. Siegel will oversee four teams: Clinical Outcome Assessment, Biomarker Qualification, Research, and Bioinformatics. Although he is now in a separate office from rheumatology, he intends to stay engaged with important issues in the field through contact with Nikolay P. Nikolov, MD, division director of rheumatology and transplant medicine, FDA.
Gordon Hutchinson, MD, Reflects on Career & Retirement
 Gordon Hutchinson, MD, FACR, associate clinical professor of medicine at Yale School of Medicine and former chief of the Section of Rheumatology at the Hospital of St. Raphael, New Haven, Conn., is renowned as both a clinician and mentor. He retired in 2020, but continues to participate in weekly grand rounds, resident conferences and once-a-month morbidity and mortality conferences.
Gordon Hutchinson, MD, FACR, associate clinical professor of medicine at Yale School of Medicine and former chief of the Section of Rheumatology at the Hospital of St. Raphael, New Haven, Conn., is renowned as both a clinician and mentor. He retired in 2020, but continues to participate in weekly grand rounds, resident conferences and once-a-month morbidity and mortality conferences.
On Tuesdays and Thursdays, Dr. Hutchinson can be found surveying and maintaining trails with the Branford Land Trust trails committee. An avid hiker, he finds the trail work “completely different, but gratifying.”
Dr. Hutchinson says he found his time as a rheumatologist very rewarding. His journey began with an undergraduate degree in biology from Fordham University, the Bronx, N.Y., and continued with medical school at the University of Zurich. While a medical student, Dr. Hutchinson recalls watching a senior physician demonstrate a clinical interaction with a rheumatology patient during history taking and exams, and thinking, “This is what I thought I would be doing.”
 From those beginnings, skillful interactions with patients became the throughline of his full career. Although the therapeutic options for patients with rheumatologic disease have expanded enormously in the last decades, the diagnosis, he believes, always depends on careful interchanges with patients rather than complete reliance on tests and imaging. “You have to listen to the patient,” Dr. Hutchinson asserts.
From those beginnings, skillful interactions with patients became the throughline of his full career. Although the therapeutic options for patients with rheumatologic disease have expanded enormously in the last decades, the diagnosis, he believes, always depends on careful interchanges with patients rather than complete reliance on tests and imaging. “You have to listen to the patient,” Dr. Hutchinson asserts.
He completed a year in Switzerland as an intern in internal medicine at Kreisspital Bülach, where he met his wife Margrit. They returned to the U.S. in 1977, and Dr. Hutchinson then interned at the Hospital of St. Raphael. While completing his rheumatology fellowship at Yale, he started the rheumatology clinic at St. Raphael’s, a clinic that served a teaching role and addressed the needs of the underserved population in New Haven. That clinic remains part of the Yale New Haven Hospital.
Dr. Hutchinson ran his clinic for 35 years, and served as chief of the Section of Rheumatology at the Hospital of St. Raphael for 29 years, garnering praise from colleagues for his diagnostic acumen and teaching abilities. He received the 2005 Teacher of the Year for the Department of Medicine for the Hospital of St. Raphael; and the Rheumatology Fellow’s Teaching and Mentoring Awards in 2005, 2016 and 2019.
Dr. Hutchinson’s wife Margit was his office manager during his entire career, so retirement has also been a dual enterprise, he noted. They are each pursuing additional interests, he in trail maintenance—“playing lumberjack!”—and she in photography, taking masters’ classes.
Sebastian E. Sattui, MD, MS, Joins UPMC as Director of Vasculitis Center
 On July 1, Sebastian E. Sattui, MD, MS, assumed an appointment as director of the University of Pittsburgh Medical Center (UPMC) Vasculitis Center. Between his rheumatology and vasculitis fellowships at Weill Cornell Medical College/Hospital for Special Surgery, New York, Dr. Sattui, who is also now assistant professor of medicine at the University of Pittsburgh School of Medicine, has spent four years preparing for this role.
On July 1, Sebastian E. Sattui, MD, MS, assumed an appointment as director of the University of Pittsburgh Medical Center (UPMC) Vasculitis Center. Between his rheumatology and vasculitis fellowships at Weill Cornell Medical College/Hospital for Special Surgery, New York, Dr. Sattui, who is also now assistant professor of medicine at the University of Pittsburgh School of Medicine, has spent four years preparing for this role.
His initial tasks at UPMC involve establishing collaborations with colleagues in other specialties to provide the multispecialty care required to secure good outcomes for patients with vasculitis and polymyalgia rheumatica (PMR). He’s also intent upon helping to streamline patients’ interface with the medical center. “It’s already hard enough [for patients to have] a complex chronic condition, even more so new patients, so we are trying to help them navigate the medical system and make the process easier and more efficient,” he says. “Our goal is to provide timely and multidisciplinary care to all patients.”
Dr. Sattui’s recent clinical research has focused on evaluating mitochondrial DNA as a measure of disease activity in vasculitis, and he will continue collaborations in that vein following wrap-up of a pilot study with colleagues at the Hospital for Special Surgery (HSS), New York, including Robert S. Spiera, MD, director of the HSS Scleroderma, Vasculitis and Myositis Center, as well as Lindsay S. Lally, MD, assistant professor of medicine at Weill Cornell Medical College.
Dr. Sattui is also focusing on research involving the compounding factors of frailty in patients with vasculitis and PMR to work toward improving the quality of life of patients living with these conditions. The overlap between frailty and these conditions will continue to be relevant, he believes, because of the age of the population affected. With his new position, there will be abundant opportunity to elucidate the effects of frailty.
He has also participated in an ACR-funded international survey of the health behaviors of people with rheumatic disease during the pandemic, which found the majority of these patients had maintained their therapy and followed public health advice to mitigate the risks of COVID-19 exposure.
Carol M. Ziminski, MD, Presented with Award for Excellence in Teaching
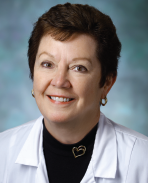 An academic rheumatologist renowned and often celebrated throughout her nearly 40-year career for her commitment to teaching, Carol M. Ziminski, MD, rates her recent award, the Professors’ Award for Excellence in Teaching to a member of the part-time faculty, high on her list of proud achievements. “I was surprised and delighted when I got the news,” she said, upon learning of the award, which was announced at the Johns Hopkins School of Medicine, Baltimore, convocation in late May.
An academic rheumatologist renowned and often celebrated throughout her nearly 40-year career for her commitment to teaching, Carol M. Ziminski, MD, rates her recent award, the Professors’ Award for Excellence in Teaching to a member of the part-time faculty, high on her list of proud achievements. “I was surprised and delighted when I got the news,” she said, upon learning of the award, which was announced at the Johns Hopkins School of Medicine, Baltimore, convocation in late May.
Also high on her list of proud career achievements is her time as the Department of Medicine’s first woman assistant chief of service, a position she held during the 1981–82 academic year. She was just past her Osler internship and residency years when the late Victor McKusick, MD, appointed her to the post. Still a rheumatology fellow at the time, Dr. Ziminski consulted her valued mentor, the late Mary Betty Stevens, MD, when making her decision to accept the appointment.
Dr. Stevens, who as the first woman director of the division of rheumatology was also a trailblazer, gave her a full endorsement. Even after she was hired as a junior faculty member, Dr. Ziminski still made it a point to round with Dr. Stevens. The latter’s ability to interact with and listen to patients became one of the through-lines in Dr. Ziminski’s own teaching methods.
The late Philip A. Tumulty, MD, was another role model, who emphasized in his book, The Effective Clinician, and his own teaching the primary importance of history taking to determine accurate diagnoses. As a core faculty member of the Vivian Thomas College’s Advisory Program, Dr. Ziminski continues to draw on the principles of listening to and observing the patient to make clinical determinations critical to diagnosis and passes on those principles to her advisees.
She says she has also benefited from the example of Antony Rosen, MD, the current director of the Division of Rheumatology, who has championed the pursuit of excellence in the division.
Dr. Ziminski was previously honored with a Hopkins Hero award upon the 125th anniversary of the institution in 2018.
She remains passionate about teaching and about rheumatology, a field which she believes is growing. This is due, in part, she notes, to the aging of the population and also to the explosion of interest and knowledge about immunology and the important pathways to disease. “The field is broad; it’s challenging and rewarding. You can make an enormous difference in people’s lives.”
Jason M. Springer, MD, MS, Now Co-Director of Vanderbilt Vasculitis Center
 Last October, in the midst of the 2020 pandemic shutdown, Jason M. Springer, MD, MS, moved from the University of Kansas Medical Center, where he was founder and director of the Vasculitis Center, to become co-director of the Vanderbilt Vasculitis Center, Nashville, Tenn. Dr. Springer, who is also associate professor of medicine in the Division of Rheumatology and Immunology in the Department of Medicine at Vanderbilt University, shares the co-directorship with Kevin W. Byram, MD.
Last October, in the midst of the 2020 pandemic shutdown, Jason M. Springer, MD, MS, moved from the University of Kansas Medical Center, where he was founder and director of the Vasculitis Center, to become co-director of the Vanderbilt Vasculitis Center, Nashville, Tenn. Dr. Springer, who is also associate professor of medicine in the Division of Rheumatology and Immunology in the Department of Medicine at Vanderbilt University, shares the co-directorship with Kevin W. Byram, MD.
There were several reasons Dr. Springer made the change from the University of Kansas. Among them, he cites the opportunity to work with Dr. Byram, whom he worked with on the ACR Vasculitis Guideline development group, and the fact that Vanderbilt has a large multistate catchment area, a wealth of research resources and a renowned rheumatology division headed by Leslie Crofford, MD.
Dr. Springer’s own path to vasculitis specialization was forged during his residency at the University of Utah, where he encountered Curry L. Koening, MD, MS, director of the Vasculitis Center. After residency, Dr. Springer followed a training path similar to his mentor, Dr. Koening, which included completing a vasculitis fellowship at Cleveland Clinic and later obtaining a Master of Science in clinical and translational research.
He moved to the University of Kansas and got involved in the Vasculitis Clinical Research Consortium. He has been a principal investigator on many clinical trials, and was co-director of the Clinical Trials Unit of the Division of Rheumatology at the University of Kansas.
In addition, he served on the Board of Directors for the Vasculitis Foundation for six years, during which time he served as the chair of the Research Committee.
Dr. Springer’s exposure to vasculitis dates back to his own family experience. Before he went to medical school, an accident revealed that his father had a neuropathy related to vasculitis. And despite aggressive treatment, his father succumbed to the disease. Because of that early exposure, Dr. Springer’s interest in vasculitis grew as he became acquainted with patients during medical school and residency.
One of the things he finds meaningful about his specialty is the opportunity to follow patients long term. “Some forms of vasculitis have changed dramatically over the years, to the point of becoming chronic instead of uniformly fatal diseases,” he says.
“I am looking forward to working with the amazing team of colleagues at Vanderbilt, and bringing a wealth of resources to the complex care of these patients.”
Gretchen Henkel is a health and medical journalist based in California.