I am not a risk taker.
I do not bungee jump.
I have never gone helicopter skiing.
I have not tried parasailing.
I always wear my seat belt.
I cross the street at the crosswalk—mostly.
And every day I make judgments that expose patients to the risk of death.
Phyllis
Phyllis, a no-nonsense professional, retired after a 40-year career in New York City and moved to Oregon to be near her children. She had severe, deforming rheumatoid arthritis (RA) and was being treated with a stable regimen of medications that included methotrexate. When I assumed her care, I adhered to a personal rule, which had served me well over two decades of practice: Never change the therapeutic combination on the first meeting if the patient perceives that it is working.
Phyllis was not taking folic acid when we first met and, consequently, I never added it to her medication mix. Although folic acid mitigates the side effects of methotrexate, it can also diminish its efficacy. Phyllis never reported any difficulty tolerating methotrexate. Over the many years that I cared for her, we tried various biologics and other approaches for her disease. I monitored her laboratory tests diligently. Phyllis’ arthritis relentlessly progressed.
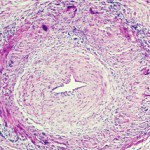
The call I received from a resident one morning produced that sinking abdominal feeling that most physicians know all too well. Phyllis had been hospitalized for aplastic anemia. The likely cause was methotrexate. Folic acid does not always prevent aplastic anemia related to methotrexate use and prescribing it with methotrexate is not a universal practice, but the studies are persuasive that it substantially reduces the likelihood of this rare toxicity. Phyllis did not recover.
Julia
Julia was a stoic, determined, active septuagenarian who rarely allowed her deforming arthritis to interfere with her vitality. Her son called me routinely one afternoon: “I can’t bring mama to her appointment tomorrow; she has the flu, no energy, and no appetite. She’s taking aspirin. I’ll let you know when she’s better.” Perhaps a few more questions might have prevented the call that came two days later. “I went to bring mama breakfast, and I found her dead in her bed.” My patient had died of a gastrointestinal hemorrhage.
The Institute of Medicine (IOM) has issued reports on how many patients have succumbed from medical errors. The IOM defines an error as “the failure of a planned action to be completed as intended … or the use of a wrong plan to achieve an aim.” An error is not the same as an adverse event, but an error is nearly the same as a preventable adverse drug event, which is one “arising because of an error.” These seemingly simple words require Talmudic interpretation. What, for example, is preventable, or how does one define a wrong plan?