 On May 6, the U.S. Food & Drug Administration’s (FDA’s) Arthritis Advisory Committee narrowly voted in support of avacopan, a C5a receptor inhibitor, for the treatment of adult patients with anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis. Although the panelists were excited about the possibility of a steroid-sparing therapy, some raised questions about whether results from the single phase 3 trial could adequately inform the risk/benefit assessment.1 The FDA will weigh the panel’s recommendation as it considers possible approval.
On May 6, the U.S. Food & Drug Administration’s (FDA’s) Arthritis Advisory Committee narrowly voted in support of avacopan, a C5a receptor inhibitor, for the treatment of adult patients with anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis. Although the panelists were excited about the possibility of a steroid-sparing therapy, some raised questions about whether results from the single phase 3 trial could adequately inform the risk/benefit assessment.1 The FDA will weigh the panel’s recommendation as it considers possible approval.
Treatment Needs for ANCA-Associated Vasculitis
ANCA-associated vasculitis is a rare, severe and sometimes fatal form of vasculitis characterized by inflammation of small vessels, often including those in the kidney. One factor that distinguishes it from other forms of vasculitis is the dominant role of neutrophils in its pathogenesis. From work in both animal and mouse models, we know activation of the alternative complement pathway plays a role in the disease pathogenesis, triggering attraction and activation of neutrophils in a complex feedback loop.1-3
Morbidity and mortality from ANCA-associated vasculitis has improved in recent decades, partly due to the introduction of new treatment regimens. The FDA approved rituximab for ANCA-associated vasculitis in 2011, and, in 2018, its label was extended to include maintenance therapy. Most patients with newly diagnosed ANCA-associated vasculitis are now started on a tapering dose of glucocorticoids, paired either with cyclophosphamide or rituximab, with a later follow-up maintenance dose of rituximab at around six months.
High doses of glucocorticoids are often used for remission induction, and they may also be employed as part of maintenance therapy, flare management and relapsing disease. This is a concern for practitioners, who hope to reduce the toxicity that results from glucocorticoid use, especially when given at high doses for prolonged periods.
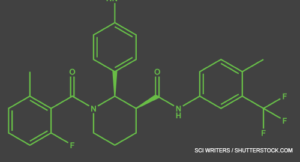
Avacopan is the first drug to be specifically developed for a vasculitis indication. Other vasculitis therapies—such as tocilizumab for giant cell arteritis or rituximab for ANCA-associated vasculitis—were first approved for other diseases. Avacopan is an oral C5a receptor antagonist that selectively blocks the effects of C5a, thus dampening neutrophil attraction and activation. It does not have FDA approval for other indications, but has orphan drug status for ANCA-associated vasculitis (specifically for microscopic polyangiitis and granulomatosis with polyangiitis) and for C3 glomerulopathy, a rare kidney disease.
Arthritis Advisory Panel Meeting
The FDA generally requires evidence from at least two adequate and well-controlled phase 3 trials to establish effectiveness of a drug. However, it exercises regulatory flexibility in certain circumstances, such as for some rare diseases. In this case, it may consider the results of a well-designed single study if the evidence is statistically persuasive and clinically meaningful.4

Dr. Jayne
Study design is a challenge for any manufacturer attempting to develop a product to potentially decrease steroid use because the FDA does not accept steroid sparing as an assessable outcome for clinical trials. For example, in the GiACTA trial, the phase 3 trial used as evidence for approval of tocilizumab for patients with giant cell arteritis, the biotechnology company Genentech wanted to give tocilizumab and demonstrate patients could then be safely taken off glucocorticoids. But the FDA required a more complicated multi-arm design.5
Other issues come up because of the way glucocorticoids have been used historically. Although they have been used for vasculitis since before drug licensing was introduced, glucocorticoids are not themselves licensed for ANCA-associated vasculitis, which brings up certain regulatory barriers in study design. Additionally, the efficacy of glucocorticoids in vasculitis to control disease activity or prevent relapse has never been officially quantified in a placebo-controlled trial.
ADVOCATE Design
For avacopan, ChemoCentryx based its application on a single phase 3 trial and two phase 2 trials.1-3 In pre-meeting documents and during the meeting itself, the company drew comparisons to the RAVE trial, used to establish the non-inferiority of rituximab to standard cyclophosphamide therapy in patients with ANCA-associated vasculitis.6 In this case, a single phase 3 trial (with supporting phase 2 data) was used as evidence for approval of rituximab.
The phase 3 trial of avacopan, ADVOCATE, used a similar, double-blind, double-dummy design.1 ADVOCATE included 331 patients with either new or relapsing ANCA-associated vasculitis. Half the participants received 30 mg of avacopan twice a day orally, as well as a prednisone placebo, out to the study’s end at 12 months. The other half received oral prednisone (tapered to 0 mg at five months) plus an avacopan placebo.

Dr. Chung
Additionally, patients received immunosuppressive treatment, either cyclophosphamide (35%) or rituximab (65%), at the discretion of the prescribing physician. Patients who had received cyclophosphamide also received follow-up azathioprine at week 15. But after initial treatment, no patients received maintenance rituximab, as would now be common practice.
Prior to enrollment, many participants were already receiving glucocorticoids as part of their treatment, to help get their disease under control. Thus, open-label prednisone treatment continued to be tapered for the early part of the trial in both groups up to the end of week 4. This had to be tapered to 20 mg or less of prednisone daily before beginning the trial, in both treatment groups.
As reported by the investigators, at week 26, the avacopan group was non-inferior to the prednisone group in terms of sustained remission. At the study’s conclusion at week 52, 66% of patients in the avacopan group were in sustained remission, as were 55% of those in the prednisone group. Thus, in terms of remission, avacopan was superior to glucocorticoids at week 52 (P=0.007).
The researchers also provided encouraging secondary endpoints related to a number of other parameters, including reduced glucocorticoid-related toxicities, fewer relapses, better quality of life measures and improvements in kidney functioning (e.g., glomerular filtration rate changes).
David R.W. Jayne, MD, a professor of clinical autoimmunity at the University of Cambridge and director of the Vasculitis and Lupus Service at Addenbrooke’s Hospital, Cambridge, England, was one of the ADVOCATE investigators and says that in the context of previous vasculitis trials, which have only rarely displayed positive effects from interventions, the ADVOCATE results are impressive.
“We’ve never seen quality-of-life benefits or [glomerular filtration rate] recovery benefits in other vasculitis trials, but we saw them consistently in this one,” says Dr. Jayne.
Criticisms & Concerns
The FDA worked with ChemoCentryx on its initial trial design. In a briefing document, the FDA noted it had previously shared many concerns with ChemoCentryx. In its pre-meeting recorded presentations and during the meeting itself, FDA representatives voiced strong criticisms of the study, raised questions about data interpretation and repeatedly called many of the results “limited” or “exploratory only.”
Throughout the hearing, the FDA seemed to subtly imply that ADVOCATE was trying to do in one trial something that it believed needed two: one demonstrating the efficacy of avacopan and a second demonstrating its capacity for steroid sparing. Looked at another way, the company was trying to demonstrate efficacy of both remission induction and remission maintenance.
Avacopan, an oral C5a receptor antagonist that selectively blocks the effects of C5a, thus dampening neutrophil attraction & activation, is the first drug to be specifically developed for a vasculitis indication.
One temporary voting member of the Advisory Committee, Sharon Chung, MD, MAS, director of the vasculitis clinic at the University of California, San Francisco, notes these double goals also posed a challenge for the committee in terms of data interpretation.
Dr. Jayne acknowledges the investigators were trying to demonstrate both avacopan’s efficacy and its capacity for steroid sparing. “In a rare disease, there are simply not enough patients to do two parallel trials, and if you are going to do sequential trials in a development program, there’s another four or five years,” he says.
Lack of Rituximab Maintenance Dose
The FDA and some committee members highlighted one key study design issue: No patients received maintenance rituximab therapy. At the time the study was designed, this indication had not been approved by the FDA, although many rheumatologists were already using rituximab in this application.
This was an intentional choice on the part of the company says Dr. Jayne, noting, “if they had redosed with rituximab at six months, … they probably wouldn’t have gotten an efficacy signal,” he explains. “The company was trying to move as close as it could to a true placebo-controlled trial. In that second six months, the steroid dose had been stopped in the steroid limb, and so it was close to an avacopan vs. placebo [trial] for that second part.”
Because the remission maintenance treatment in the rituximab arm does not reflect current standard of care, Dr. Chung notes, she can’t tell her patients how the risk of relapse with avacopan compares with the risk of relapse with rituximab when used for remission maintenance.
Non-Study Supplied Glucocorticoids
The FDA representatives and some committee members also raised concerns about the use of glucocorticoids in the study. In addition to the study-supplied glucocorticoids (in the prednisone group), many of the participants received additional glucocorticoids as part of tapering from their initial management, as a premedication (in the rituximab group) or for other indications.
‘We saw signs of efficacy in this study, but confounding factors put into question the degree of efficacy.’ —Dr. Chung
Most of the additional glucocorticoids were given in the first half of the study: 86% of the subjects given avacopan used glucocorticoids at some point during the first 26 weeks. However, the mean cumulative glucocorticoid dose per patient was considerably lower in the avacopan group compared to the dose in the prednisone-treated patients (1,349 mg vs. 3,655 mg).
The FDA criticized this, saying the investigators could not rightfully claim non-inferiority at six months because both treatment groups had had some steroid use. Dr Jayne notes, “It was not easy to fully defend against that, except to say that with avacopan you got by with much less steroid.”
Statistical Analyses
The FDA also contested the actual numbers and resulting statistical significance. The investigators had used a blinded adjudication committee to help get the most accurate data possible in terms of their endpoint analyses using the Birmingham Vasculitis Activity Score (BVAS). Potential issues that might have led to data scoring problems were predefined. This is standard practice in vasculitis and lupus trials because the available scoring tools can be difficult to use 100% consistently across investigators, in terms of their ability to accurately detect current disease activity.
The FDA representatives reran statistical analyses using the original scores of the investigators, claiming they “might be more reflective of real-world use.” For these data that had not been cleaned up by blinded adjudicators, the endpoint of remission at week 26 and sustained remission at week 52 didn’t change. But using this other dataset, the endpoint of superiority at week 52 no longer reached statistical significance, raising questions for some about the drug’s true efficacy.
Subgroup analyses also posed thorny questions. The patients receiving rituximab vs. cyclophosphamide were distributed equally between the avacopan and prednisone groups as part of the trial design. But the FDA and some panel members expressed reservations that when response to avacopan was analyzed by subgroup, the patients who had received cyclophosphamide (plus, later, azathioprine) had not shown overall treatment superiority (in contrast to analyses of the rituximab group or analyses including all patients).
However, it is important to note the trial was not designed to pick up such differences in terms of its statistical power, and differences in rituximab vs. cyclophosphamide may reflect other factors, such as the part of the world where they were prescribed.
Safety Signals
The FDA also highlighted some potential safety concerns, especially with respect to potential toxicity in the liver. Nine patients in the avacopan group had abnormalities on liver-function testing, some of which led to drug discontinuation, compared with six in the prednisone group. All these abnormalities resolved after drug withdrawal.
The investigators responded that these patients were on several different drugs that might have induced these liver issues, including cyclophosphamide and trimethoprim-sulfamethoxazole, so attributing these to avacopan may be shortsighted. Of more theoretical concern is the fact that the total drug exposure is only about 400 patients (across the ADVOCATE phase 3 study and the two phase 2 studies).1-3
One key difference between the ADVOCATE and RAVE trials, says Dr. Chung, is that rituximab had already been approved for other diseases and had established a much more extensive safety profile. “The limited experience with avacopan makes it challenging to unequivocally endorse approval of this new drug,” she adds.
Vote
On the question of whether the efficacy data supported approval of avacopan for adult patients with ANCA-associated vasculitis, the committee split 9–9. The committee voted 10–8 that avacopan’s safety profile adequately supported its approval. For the final question, whether the overall benefit-risk profile supported avacopan approval, the vote was also 10–8 in favor.
Given this lack of consensus, it may have been a difficult vote for many of the committee members. The rheumatology community had been quite excited by the prospect of the new drug, and a favorable editorial in The New England Journal of Medicine had sparked much interest.7
“There was, in some respects, an emotional drive to have this drug approved,” Dr. Chung says. “We saw signs of efficacy in this study, but confounding factors put into question the degree of efficacy. Yet we all know that we need an alternative for glucocorticoids, given their significant toxicity.”
The FDA will consider the recommendations of the Arthritis Advisory Committee as it continues to contemplate avacopan’s potential approval, but it is not required to follow them. A final decision by the FDA is expected soon.
Ruth Jessen Hickman, MD, is a graduate of the Indiana University School of Medicine. She is a freelance medical and science writer living in Bloomington, Ind.
3 New Guidelines for Vasculitis
In July, the ACR in concert with the Vasculitis Foundation released three new guidelines for: ANCA-associated vasculitis, giant cell arteritis and Takayasu arteritis, and polyarteritis nodosa. Read our summary article or access the full guideline articles. A guideline for Kawasaki disease is anticipated later this year.
Late-breaking news
On July 6, ChemoCentryx announced it had filed an amendment to its new drug application to address some of the concerns raised in the Advisory Committee meeting. This has delayed the FDA’s final decision, which is now expected in October.
References
- Jayne DRW, Merkel PA, Schall TJ, et al. Avacopan for the treatment of ANCA-associated vasculitis. N Engl J Med. 2021 Feb 18;384(7):599–609.
- Merkel PA, Niles J, Jimenez R, et al. Adjunctive treatment with avacopan, an oral C5a receptor inhibitor, in patients with antineutrophil cytoplasmic antibody-associated vasculitis. ACR Open Rheumatol. 2020;2(11):662–671.
- Jayne DRW, Bruchfeld AN, Harper L, et al. Randomized trial of C5a receptor inhibitor avacopan in ANCA-associated vasculitis. J Am Soc Nephrol. 2017 Sep;28(9):2756–2767.
- U.S. Department of Health and Human Services. Food and Drug Administration. Demonstrative substantial evidence of effectiveness for human drug and biological products: Guidance for industry. 2019.
- Stone JH, Tuckwell K, Dimonaco S, et al. Trial of tocilizumab in giant-cell arteritis. N Engl J Med. 2017 Jul 27;377(4):317–328.
- Stone JH, Merkel PA, Spiera R, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010 Jul 15;363(3):221–232.
- Warrington KJ. Avacopan—time to replace glucocorticoids? N Engl J Med. 2021 Feb 18;384(7):664–665.



