The rupture of aneurysms in Takayasu’s arteritis can be catastrophic and, unlike atherosclerotic aneurysms, size may not be the only consideration for surgery.
Image Credit: BioMedical/shutterstock.com
A healthy 30-year-old Indian male was performing his routine workout in the gym when he developed giddiness and transient blackouts. He thought it was due to exercising excessively. Over the next month, he developed a low-grade fever and started feeling lethargic, to the extent that he was unable to exercise or work.
He was admitted to the hospital with the above complaints and was found to be hypertensive. Investigatory reports showed elevated inflammatory markers with an erythrocyte sedimentation rate (ESR) of 100 mm/hour and C-reactive protein (CRP) of 96 mg/dL. An ultrasound study of the abdomen showed a shrunken left kidney and altered Doppler signals emanating from the proximal left renal artery suggestive of renal artery stenosis.
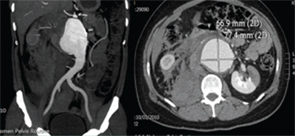
Figure 1. CT-angiography showing ruptured abdominal aortic aneurysm with a retroperitoneal and intraperitoneal hematoma with left renal infarct.
CT-aortography demonstrated an abdominal aortic aneurysm extending from the origin of the superior mesenteric artery (SMA) to the aortic bifurcation and measuring 11.9 cm in length and 4 cm in width. The origins of both renal arteries were involved in the aneurysm. There was focal ectasia of both carotid bulbs and dilation and stenosis of both subclavian arteries at their origins. Mild aneurismal dilation of the left distal external iliac and left femoral artery was seen. A PET-CT showed active inflammation involving the aortic arch, origin of the left common carotid, ascending aorta, both carotid and femoral arteries. He was diagnosed with Takayasu’s arteritis (TA), and he was treated with prednisolone 60 mg/day and methotrexate 15 mg/week. Over the course of one year, he had a good response to treatment, and the steroids were tapered slowly to 5 mg/day. He discontinued therapy and did not keep future appointments.
A year later, he presented to the emergency department with acute abdominal pain and hypotension. Imaging confirmed a ruptured aortic aneurysm with a retroperitoneal and intraperitoneal hematoma. There was extensive infarction of the left kidney (see Figure 1, left). His echocardiogram showed dilation of the aortic root (3.6 cm) with an aneurysm of the sinus of Valsalva. He underwent emergency surgical repair of the aortic aneurysm using a Dacron graft. Post-surgery, he had temporary renal shutdown, which necessitated short-term hemodialysis. He recovered well and was maintained on prednisolone and methotrexate for another four years. Serial ESR and CRP levels conducted between 2010 and 2014 were in the normal range.
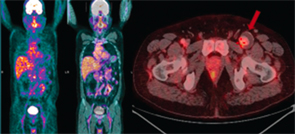
Figure 2. PET-CT showing low to moderate inflammatory activity with aneurismal dilation of the left common femoral artery with thrombus.
In 2014, a repeat PET-CT showed low to moderate inflammatory activity with aneurysmal dilation of the left common femoral artery (see Figure 2). He was advised to have surgery for the aneurysm after a period of increased immunosuppression. Six months later, he underwent left common femoral artery and superficial femoral artery aneurysm excision, with external iliac artery to superficial femoral artery interposition grafting (see Figures 3 and 4). Histologically, the aneurysmal segment showed disorganization of the elastic lamina of the media, with inadequate supportive fibrous tissue, and a large intraluminal thrombus (see Figure 5).
Four months following the surgery, he is stable and able to resume his normal activities.
Key points of this presentation:
- Although arterial narrowing is classical, aneurysms in TA are an important complication, and they can occur at multiple sites;
- Patients need regular monitoring, even if they are asymptomatic, because aneurysms can progress despite normal values of inflammatory markers and PET-CTs showing low disease activity;
- Rupture of these aneurysms can be catastrophic and, unlike atherosclerotic aneurysms, size may not be the only consideration for surgery;
- Timely surgical repair of aneurysms yields good results; and
- Patient education regarding the continuation of medication and regular follow-up are very important.
Discussion
Takayasu’s arteritis (TA) is a large-vessel arteritis commonly described in young Asians. It involves the aorta and its branches, with stenosis more commonly seen than aneurysms. In a large number of patients, the disease progresses without any symptoms until critical ischemia results in symptoms of claudication. Any part of the aorta can be involved, and the most commonly affected branches are the subclavian and common carotid arteries.1,2 Stenotic lesions are found in >90% of patients, whereas aneurysms are reported in approximately 25%.2 Stenotic lesions and aneurysms are associated with considerable morbidity and mortality. The consequences of TA are often severe, with 74% of patients reporting considerably compromised daily activities and 23% of patients unable to work.2
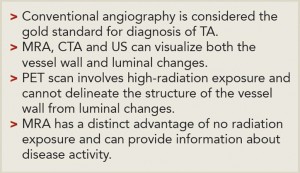
Disease monitoring is a great challenge to the treating physician because there are no markers, which can reliably predict disease activity. Inflammatory markers are notoriously fallacious in assessing disease activity. High-resolution ultrasound (US), magnetic resonance angiography (MRA), CT angiography (CTA) and PET have been used for diagnosis and monitoring disease activity (see Table 1). However, there still is no consensus on which imaging modality should be routinely used.
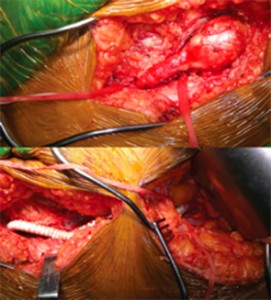
Figure 3. Intraoperative images showing femoral artery aneurysm (top) and Dacron graft after resection (bottom).
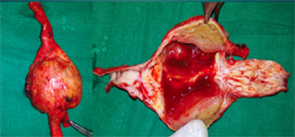
Figure 4. Surgical specimen showing aneurismal dilation and thrombus.
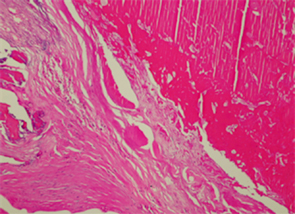
Figure 5. Histopathology image showing intraluminal thrombus with disorganized elastic lamina of the media and scanty inflammatory infiltrate.
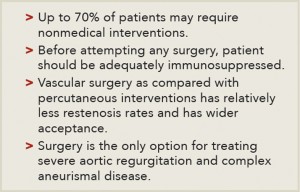
Surgical treatment should be done only after adequately treating with immunosuppressive medications (see Table 2). Surgical indications include severe uncontrolled renovascular hypertension, coarctation of the aorta, severe cerebral ischemia, severe aortic regurgitation and progressive aneurismal enlargement or dissection. Surgical bypass procedures have good long-term survival rates, with restenosis rates being less than 30%.3,4 The surgical procedures can be done either by open procedures or through endovascular approach with the use of either autologous or synthetic grafts.
Back to the Case
Our patient had aneurysms at more than one site. There was rapid worsening of the aortic aneurysm leading to rupture. He was fortunate to have survived that and improved after an extensive emergency surgery. Although the femoral artery aneurysm was asymptomatic, because it was reasonably large and had the potential to rupture, elective surgery was done after a six-month period of escalated immunosuppression.
G.C. Yathish, MD, is a rheumatology DNB student at Hinduja Hospital in Mumbai, India.
Taral Parikh, MD, is a rheumatology DNB student at Hinduja Hospital in Mumbai, India.
Parikshit Sagdeo, MD, is a rheumatology DNB student at Hinduja Hospital in Mumbai, India.
Balakrishnan Canchi, MD, is the chief of rheumatology at Hinduja Hospital in Mumbai, India.
Gurmeet Mangat, MD, is a consultant rheumatologist at Hinduja Hospital in Mumbai, India.
Hemanth Kumar Pandharpurkar, MS, is a consultant vascular surgeon at Hinduja Hospital in Mumbai, India.
References
- Jain S, Kumari S, Ganguly NK, et al. Current status of Takayasu arteritis in India. Int J Cardiol. 1996 Aug;54 Suppl:S111–S116.
- Kerr GS, Hallahan CW, Giordano J, et al. Takayasu arteritis. Ann Intern Med. 1994 Jun 1;120(11):919–929.
- Liang P, Hoffman GS. Advances in the medical and surgical treatment of Takayasu arteritis. Curr Opin Rheumatol. 2005 Jan;17(1):16–24.
- Miyata T, Sato O, Koyama H, et al. Long-term survival after surgical treatment of patients with Takayasu’s arteritis. Circulation. 2003 Sep 23;108(12):1474–1480.