Laboratory Results
Laboratory tests confirmed raised markers for inflammation and thrombocytosis. Testing for human leukocyte antigen (HLA) B27, sent from the other hospital, returned positive. Further laboratory workup revealed negative occult fecal blood, and his stool culture was negative for Campylobacter, Enterohemorrhagic E. coli, Salmonella, Shigella, and Yersinia.
The diagnosis of a reactive arthritis (ReA) was made and the patient was prescribed prednisone 60 mg daily. His fevers quickly resolved, and over the next few weeks his arthritis improved. Although he had some swelling of the ankles and the dorsum of the feet, he was able to resume playing soccer. Repeat bloodwork four weeks later showed a normalization of blood counts and inflammatory markers. One month later, sulfasalazine 1,000 mg twice daily was prescribed and prednisone was weaned and discontinued. The arthritis completely resolved within a few months, and he continues to do well without disease recurrence.
Discussion
Take-Home Points
- The differential diagnosis of fever and arthritis is fairly limited in children and adults.
- ReA usually occurs one to four weeks after gastrointestinal or genitourinary infection.
- ReA presents with painful arthritis predominantly affecting lower extremites, and can cause enthesitis, dactylitis, and systemic symptoms.
- ReA is most often caused by Chlamydial infections in adults, while gastrointestinal infections are the most common cause of ReA in children.
- ReA and the spondylarthropathies appear to fall within the spectrum of the polygenic autoinflammatory diseases.
- Treatment may include NSAIDs, DMARDs, systemic corticosteroids, and biologics for recalcitrant disease.
- Prognosis is good, although the presence of HLA-B27 may raise the risk for severe disease and a more chronic course.
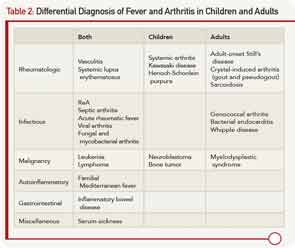
The presence of arthritis and fever has a fairly limited differential diagnosis in children and adults, and a comprehensive, expedited evaluation should take place to avoid the potential morbidity and mortality of some important diseases. The differential diagnosis is listed in Table 2. The age of onset, pattern of fever, type and number of joints involved, associated symptoms, laboratory testing, and synovial fluid analysis may lead to the diagnosis.
Traditionally, ReA is diagnosed by using the Berlin Third International Workshop on Reactive Arthritis criteria (1995) shown in Table 3.1 Criteria include an asymmetric oligoarthritis, predominantly involving the lower limbs, and clinical or laboratory evidence of a preceding infection with enteric or genitourinary organisms including Chlamydia trachomatis, Shigella, Salmonella, Yersinia, and Campylobacter. Nevertheless, recent reports have also implicated atypical organisms as causative agents of ReA, including Giardia lambia and Clostridium difficile, as well as intravesical Bacillus Calmette-Guerin therapy for bladder cancer.2,3


